Monoamine releasing agent

A monoamine releasing agent (MRA), or simply monoamine releaser, is a drug that induces the release of one or more monoamine neurotransmitters from the presynaptic neuron into the synapse, leading to an increase in the extracellular concentrations of the neurotransmitters and hence enhanced signaling by those neurotransmitters.[2][3][4][1][5] The monoamine neurotransmitters include serotonin, norepinephrine, and dopamine; MRAs can induce the release of one or more of these neurotransmitters.[2][3][4][1][5]
MRAs work by reversing the direction of the monoamine transporters (MATs), including the serotonin transporter (SERT), norepinephrine transporter (NET), and/or dopamine transporter (DAT), causing them to promote efflux of non-vesicular cytoplasmic monoamine neurotransmitter rather than reuptake of synaptic monoamine neurotransmitter.[5][6][1][7] Many, but not all MRAs, also reverse the direction of the vesicular monoamine transporter 2 (VMAT2), thereby additionally resulting in efflux of vesicular monoamine neurotransmitter into the cytoplasm.[5]
A variety of different classes of drugs induce their effects in the body and/or brain via the release of monoamine neurotransmitters.[2][3] These include psychostimulants and appetite suppressants acting as dopamine and norepinephrine releasers like amphetamine, methamphetamine, and phentermine; sympathomimetic agents acting as norepinephrine releasers like ephedrine and pseudoephedrine; non-stimulant appetite suppressants acting as serotonin releasers like fenfluramine and chlorphentermine; and entactogens acting as releasers of serotonin and/or other monoamines like MDMA.[2][3] Trace amines like phenethylamine and tryptamine, as well as the monoamine neurotransmitters themselves, are endogenous MRAs.[2][3][4] It is thought that monoamine release by endogenous mediators may play some physiological regulatory role.[4]
MRAs must be distinguished from monoamine reuptake inhibitors (MRIs) and monoaminergic activity enhancers (MAEs), which similarly increase synaptic monoamine neurotransmitter levels and enhance monoaminergic signaling but work via distinct mechanisms.[5][1][8][9]
Types and selectivity
[edit]MRAs can be classified by the monoamines they mainly release, although these drugs lie on a spectrum:[2][3][4][5]
- Selective for one neurotransmitter
- Serotonin releasing agent (SRA) (e.g., chlorphentermine, MMAI)
- Norepinephrine releasing agent (NRA) (e.g., ephedrine, pseudoephedrine)
- Dopamine releasing agent (DRA) (no known examples)
- Non-selective, releasing two or more neurotransmitters
- Norepinephrine–dopamine releasing agent (NDRA) (e.g., amphetamine, methamphetamine)
- Serotonin–norepinephrine releasing agent (SNRA) (e.g., fenfluramine, MDAI)
- Serotonin–dopamine releasing agent (SDRA) (e.g., 5-chloro-αMT)
- Serotonin–norepinephrine–dopamine releasing agent (SNDRA) (e.g., MDMA)
The differences in selectivity of MRAs is the result of different affinities as substrates for the monoamine transporters, and thus differing ability to gain access into monoaminergic neurons and induce monoamine neurotransmitter release.
As of present, no selective DRAs are known. This is because it has proven extremely difficult to separate DAT affinity from NET affinity and retain releasing efficacy at the same time.[10] Several selective SDRAs, including tryptamine, (+)-α-ethyltryptamine (αET), 5-chloro-αMT, and 5-fluoro-αET, are known.[11][12] However, besides their serotonin release, these compounds additionally act as non-selective serotonin receptor agonists, including of the serotonin 5-HT2A receptor (with accompanying hallucinogenic effects), and some of them are known to act as monoamine oxidase inhibitors.[11][12]
Effects and uses
[edit]MRAs can produce varying effects depending on their selectivity for inducing the release of different monoamine neurotransmitters.[3]
Selective SRAs such as chlorphentermine have been described as dysphoric and lethargic.[13][14] Less selective SRAs that also stimulate the release of dopamine, such as methylenedioxymethamphetamine (MDMA), are described as more pleasant, more reliably elevating mood and increasing energy and sociability.[15] SRAs have been used as appetite suppressants and as entactogens. They have also been proposed for use as more effective antidepressants and anxiolytics than selective serotonin reuptake inhibitors (SSRIs) because they can produce much larger increases in serotonin levels in comparison.[16]
DRAs, usually non-selective for both norepinephrine and dopamine, have psychostimulant effects, causing an increase in energy, motivation, elevated mood, and euphoria.[17] Other variables can significantly affect the subjective effects, such as infusion rate (increasing positive effects of DRAs) and psychological expectancy effects.[18] They are used in the treatment of attention deficit hyperactivity disorder (ADHD), as appetite suppressants, wakefulness-promoting agents, to improve motivation, and are drugs of recreational use and misuse.
Selective NRAs are minimally psychoactive, but as demonstrated by ephedrine, may be distinguished from placebo, and may trends towards liking.[19] They may also be performance-enhancing,[20] in contrast to reboxetine which is solely a norepinephrine reuptake inhibitor.[21][22] In addition to their central effects, NRAs produce peripheral sympathomimetic effects like increased heart rate, blood pressure, and force of heart contractions. They are used as nasal decongestants and bronchodilators, but have also seen use as wakefulness-promoting agents, appetite suppressants, and antihypotensive agents. They have additionally seen use as performance-enhancing drugs, for instance in sports.
Mechanism of action
[edit]MRAs cause the release of monoamine neurotransmitters by various complex mechanisms of action. They may enter the presynaptic neuron primarily via plasma membrane transporters, such as the dopamine transporter (DAT), norepinephrine transporter (NET), and serotonin transporter (SERT). Some, such as exogenous phenethylamine, amphetamine, and methamphetamine, can also diffuse directly across the cell membrane to varying degrees. Once inside the presynaptic neuron, they may inhibit the reuptake of monoamine neurotransmitters through vesicular monoamine transporter 2 (VMAT2) and release the neurotransmitters stores of synaptic vesicles into the cytoplasm by inducing reverse transport at VMAT2. MRAs can also bind to the intracellular receptor TAAR1 as agonists, which triggers a phosphorylation cascade via protein kinases that results in the phosphorylation of monoamine transporters located at the plasma membrane (i.e., the dopamine transporter, norepinephrine transporter, and serotonin transporter); upon phosphorylation, these transporters transport monoamines in reverse (i.e., they move monoamines from the neuronal cytoplasm into the synaptic cleft).[23] The combined effects of MRAs at VMAT2 and TAAR1 result in the release of neurotransmitters out of synaptic vesicles and the cell cytoplasm into the synaptic cleft where they bind to their associated presynaptic autoreceptors and postsynaptic receptors. Certain MRAs interact with other presynaptic intracellular receptors which promote monoamine neurotransmission as well (e.g., methamphetamine is also an agonist at σ1 receptor).
In spite of some findings that TAAR1 activation by amphetamines can reverse the monoamine transporters and mediate monoamine release however,[23][24][25][26] major literature reviews on MRAs by recognized experts like on these agents Richard B. Rothman and David J. Heal state that the nature of monoamine transport reversal is not well understood and/or do not mention TAAR1 activation.[5][6][1][7] Moreover, amphetamines continue to induce dopamine and norepinephrine release in in-vitro systems lacking the TAAR1, like HEK293 cells,[27] and produce monoamine release and psychostimulant-like effects in TAAR1 knockout mice.[23][28][29][30][31] In fact, TAAR1 knockout mice are supersensitive to the effects of amphetamines, and TAAR1 activation appears to inhibit the striatal dopaminergic actions of psychostimulants.[23][29][28][30][31] Additionally, numerous substrate-type MRAs that do not bind to and/or activate the (human) TAAR1 are known, including most cathinones, ephedrine, 4-methylamphetamine (4-MA), para-methoxyamphetamine (PMA), 4-methylthioamphetamine (4-MTA), MBDB, MDEA, 5-APDB, 5-MAPDB, meta-chlorophenylpiperazine (mCPP), TFMPP, 4-methylaminorex derivatives, and methylhexanamine, among others.[32][33][34][35] In addition, amphetamine and methamphetamine themselves only activate the human TAAR1 at micromolar concentrations and with potency an order of magnitude lower than phenethylamine.[34] However, there is indication that TAAR1, although non-essential for induction of monoamine release, might augment the releasing potency of amphetamines as dopamine releasing agents, at least in vitro.[26]

There is a constrained and relatively small molecular size requirement for compounds to act as MRAs.[5] This is because they must be small enough to serve as substrates of the monoamine transporters and thereby be transported inside of monoaminergic neurons by these proteins, in turn allowing them to induce monoamine neurotransmitter release.[5] Compounds with chemical features extending beyond the size constraints for releasers will instead act as partial releasers, reuptake inhibitors, or be inactive.[5] Partial releasers show reduced maximal efficacy in releasing monoamine neurotransmitters compared to conventional full releasers.[5]
Other related agents
[edit]DAT "inverse agonists"
[edit]Dopamine reuptake inhibitors (DRIs) have been grouped into two types, typical or conventional DRIs like cocaine, WIN-35428 (β-CFT), and methylphenidate that produce potent psychostimulant, euphoric, and reinforcing effects, and atypical DRIs like vanoxerine (GBR-12909), modafinil, benztropine, and bupropion, which do not produce such effects or have greatly reduced such effects.[7][6][5][36] It has been proposed that typical DRIs may not actually be acting primarily as DRIs but rather as dopamine releasing agents (DRAs) via mechanisms distinct from conventional substrate-type DRAs like amphetamines.[7] A variety of different pieces of evidence support this hypothesis and help to explain otherwise confusing findings.[7] Under this model, typical cocaine-like DRIs have been referred to with the new label of dopamine transporter (DAT) "inverse agonists" to distinguish them from conventional substrate-type DRAs.[7] An alternative theory is that typical DRIs and atypical DRIs stabilize the DAT in different conformations, with typical DRIs resulting in an outward-facing open conformation that produces differing pharmacological effects from those of atypical DRIs.[6][5][36][37]
Monoaminergic activity enhancers
[edit]Some MRAs, like the amphetamines amphetamine and methamphetamine, as well as trace amines like phenethylamine, tryptamine, and tyramine, are additionally monoaminergic activity enhancers (MAEs).[8][9][38] That is, they induce the action potential-mediated release of monoamine neurotransmitters (in contrast to MRAs, which induce uncontrolled monoamine release independent of neuronal firing).[8][9][38] They are usually active as MAEs at much lower concentrations than those at which they induce monoamine release.[8][9][38] The MAE actions of MAEs may be mediated by TAAR1 agonism, which has likewise been implicated in monoamine-releasing actions.[39][40] MAEs without concomitant potent monoamine-releasing actions, like selegiline (L-deprenyl), phenylpropylaminopentane (PPAP), and benzofuranylpropylaminopentane (BPAP), have been developed.[8][9]
Endogenous MRAs
[edit]A number of endogenous compounds are known to act as MRAs.[4][41][42][11][5] These include the monoamine neurotransmitters dopamine (an NDRA),[41] norepinephrine (an NDRA),[41] and serotonin (an SRA) themselves,[41] as well as the trace amines phenethylamine (an NDRA),[5][38][43][44] tryptamine (an SDRA or imbalanced SNDRA),[42][11] and tyramine (an NDRA).[41][4] Synthetic MRAs are substantially based on structural modification of these endogenous compounds, most prominently including the substituted phenethylamines and substituted tryptamines.[41][2][3][42][45][46][47]
Release of monoamine neurotransmitters by themselves, for instance in the cases of serotonin, norepinephrine, and dopamine, has been referred to as "self-release".[4] The physiological significance of the findings that monoamine neurotransmitters can act as releasing agents of themselves is unclear.[4] However, it could imply that efflux is a common neurotransmitter regulatory mechanism that can be induced by any transporter substrate.[4]
It is possible that monoamine neurotransmitter self-release could be a protective mechanism.[4][48] It is notable in this regard that intracellular non-vesicular or cytoplasmic dopamine is toxic to neurons and that the vesicular monoamine transporter 2 (VMAT2) is neuroprotective by packaging this dopamine into synaptic vesicles.[49][50][51][48] Along similar lines, MRAs induce the efflux of non-vesicular monoamine neurotransmitter and thereby move cytoplasmic neurotransmitter into the extracellular space.[5] On the other hand, many MRAs but not all also act as VMAT2 inhibitors and reversers, and hence concomitantly induce the release of vesicular monoamine neurotransmitters like dopamine into the cytoplasm.[5] Induction of VMAT2 efflux by MRAs appears to be related to their monoaminergic neurotoxicity.[52][53][54]
Monoaminergic neurotoxicity
[edit]Some MRAs have been found to act as monoaminergic neurotoxins and hence to produce long-lasting damage to monoaminergic neurons.[55][56] Examples include dopaminergic neurotoxicity with amphetamine and methamphetamine and serotonergic neurotoxicity with methylenedioxymethamphetamine (MDMA).[55][56] Amphetamine may produce significant dopaminergic neurotoxicity even at therapeutic doses.[57][58][59][60][61][62] However, clinical doses of amphetamine producing neurotoxicity is controversial and disputed.[63][57][59] In contrast to amphetamines, monoamine reuptake inhibitors like methylphenidate lack apparent neurotoxic effects.[57]
Analogues of MDMA with retained MRA activity but reduced or no serotonergic neurotoxicity, like 5,6-methylenedioxy-2-aminoindane (MDAI) and 5-iodo-2-aminoindane (5-IAI), have been developed.[64][65] Certain drugs have been found to block the neurotoxicity of MRAs in animals.[56] For instance, the selective MAO-B inhibitor selegiline has been found to prevent the serotonergic neurotoxicity of MDMA in rodents.[56]
Chemical families
[edit]MRAs are usually arylalkylamines. A number of different structural families of compounds have been found to act as MRAs. The possible structural forms of MRAs are limited by a small molecular size requirement for activity.[5] Molecules that are too large become monoamine reuptake inhibitors as they can no longer be transported into neurons by the monoamine transporters and induce monoamine release intracellularly.[5]
Phenethylamine-like
[edit]- Phenethylamines (2-phenylethylamines) (e.g., phenethylamine, tyramine, dopamine, norepinephrine)
- Amphetamines (α-methylphenethylamines) (e.g., amphetamine, methamphetamine, fenfluramine)
- Cathinols (β-hydroxyamphetamines) (e.g., phenylpropanolamine, ephedrine, pseudoephedrine, cathine)
- Cathinones (β-ketoamphetamines) (e.g., cathinone, methcathinone, mephedrone)
- Phentermines (α-methylamphetamines) (e.g., phentermine, mephentermine, chlorphentermine, clortermine)
- Phenylisobutylamines (α-ethylphenethylamines) (e.g., phenylisobutylamine, 4-CAB, 4-MAB, buphedrone)
- Ring-extended amphetamines
- Benzodioxolylaminopropanes (methylenedioxyamphetamines) (e.g., MDA, MDMA, MDEA, methylone)
- Benzodioxanylaminopropanes (ethylenedioxyamphetamines) (e.g., EDA, EDMA, EDA-2, IDA, EDMC)[67][68][69]
- Benzofuranylaminopropanes (e.g., 5-APB, 5-MAPB, 6-APB, 6-MAPB, 5-APDB, 5-MAPDB, 6-APDB, 6-MAPDB, IBF5MAP)[70][71][72]
- Benzothiophenylaminopropanes (e.g., 4-APBT, 5-APBT, 5-MAPBT, 6-APBT, 7-APBT)[74]
- Benzothiazolylaminopropanes (5-BZT-MDMA, 6-BZT-MDMA)[75]
- Indolylaminopropanes (e.g., 5-IT/5-API, 6-IT/6-API)[76]
- Indanylaminopropanes (e.g., 5-APDI/IAP, 5-MAPDI)[72][77]
- Naphthylaminopropanes (e.g., NAP, methamnetamine/MNAP, ENAP, BMAPN)[78][79]
- Tetralinylaminopropanes (e.g., 6-APT/TAP)[72]
- Other ring-extended amphetamines (e.g., ODMA,[80] SeDMA,[80] TDMA[80])
- Amphetamines (α-methylphenethylamines) (e.g., amphetamine, methamphetamine, fenfluramine)
- Cyclopentanylaminopropanes (e.g., cyclopentamine)
- Cyclohexylaminopropanes (e.g., norpropylhexedrine, propylhexedrine)
- Phenylpropylamines (e.g., phenylpropylamine)[81][4]
- Thiophenylisopropylamines (e.g., thiopropamine, methiopropamine, thiothinone)
- Phenylalkenylamines and phenylalkynylamines (e.g., phenylbutynamine, phenylbutenamine)[82][83][78]
- Other possible groups (e.g., 2-furylethylamines, 2-tetrahydrofurylethylamines, 2-pyrrolylethylamines)[47]
Amine fused into ring
[edit]- Phenylalkylpyrrolidines (e.g., α-PPP, 4-MePPP)[84][85]
- Phenylmorpholines (e.g., phenmetrazine, phendimetrazine)
- Methylenedioxyphenylmorpholines (e.g., 3-MDPM)
- Naphthylmorpholines (e.g., naphthylmorpholine, naphthylmetrazine)
- Phenyloxazolamines (e.g., aminorex, 4-methylaminorex, pemoline)
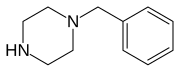
- Benzylpiperazines (e.g., 1-benzylpiperazine, MBZP)
- Benzylpiperidines (e.g., 4-benzylpiperidine)
- Phenylpiperazines (e.g., 1-phenylpiperazine, mCPP, TFMPP, oMPP, pFPP, pMeOPP)[86]
Alkyl chain fused into ring
[edit]- 2-Aminoindanes (e.g., 2-aminoindane, NM-2-AI, MMAI, MEAI, ETAI, TAI, 5-IAI)[87][88][79]
- 2-Aminotetralins (e.g., 2-aminotetralin, 6-CAT)[88][79]
- Other possible groups (e.g., 2-amino-1,2-dihydronaphthalenes,[90][91] aminobenzocycloheptenes[79][92])
Tryptamine-like
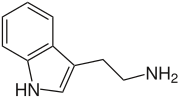
[edit]- Tryptamines (2-(3-indolyl)ethylamines) (e.g., tryptamine, serotonin, bufotenin, DMT, psilocin)[42][11]
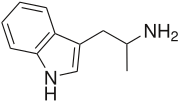
- α-Alkyltryptamines (e.g., αMT (3-API), αET, 5-chloro-αMT, 5-fluoro-αMT)[11][66]
- β-Keto-α-alkyltryptamines (e.g., BK-NM-AMT, BK-5F-NM-AMT)[93][94]
- α-Alkyltryptamines (e.g., αMT (3-API), αET, 5-chloro-αMT, 5-fluoro-αMT)[11][66]
- Isotryptamines (2-(1-indolyl)ethylamines) (e.g., isoAMT)[12]
- Benzothiophenylaminopropanes (e.g., 2-APBT, 3-APBT)[74]
- Benzofuranylaminopropanes (e.g., 2-APB, 2-MAPB, 3-APB, 3-MAPB)[71]
- Other possible groups (e.g., 2-pyrrolylethylamines)[47]
Ring-less (alkylamines)
[edit]- Alkylamines (e.g., 1,3-DMBA,[27] 1,4-DMAA,[27][95] heptaminol,[96][97] iproheptine, isometheptene,[96] methylhexanamine/1,3-DMAA,[27][52][95][98] octodrine,[27][99] oenethyl,[100][101] tuaminoheptane[27][96][102][97])[100]
Chemical family structures gallery
[edit]Activity profiles
[edit]The activities of many MRAs in terms of their potencies, efficacies, and selectivities for monoamine release induction in vitro have been characterized in numerous studies in the scientific literature.[2][103][3][5][104] These studies have been especially conducted by the research lab led by Richard B. Rothman and Michael H. Baumann at the National Institute on Drug Abuse (NIDA).[2][103][3][104] These researchers developed an assay measuring monoamine release from rat brain synaptosomes in 1999 that has subsequently been widely employed.[104][103][41][105][106] The data with this procedure from many relevant studies are provided in the table below.[2][3] The Rothman and Baumann lab refers to these data as the "Phenyl Amine Library", "Phenethylamine Library", "Phenylethylamine Library", or "PAL" library, a large library of values of phenethylamine analogs at the monoamine transporters, and has designated PAL-# code names for the drugs included in it.[107][5][104]
Another method of measuring monoamine release involves the use of human HEK293 cells transfected with and expressing monoamine transporters.[108][109][64][110][67] However, MRAs show differing and much lower potencies in this system compared to rat brain synaptosomes, and it is much less frequently employed.[108][109][64][110][67] The reasons for these differences are not entirely clear, but may be related to species differences, differences in release assay methods, and/or absence of important neuronal membrane proteins in non-neuronal HEK293 cells.[67][26] One possible difference in terms of the use of non-neuronal cells may be that TAAR1 is present in rat brain synaptosomes but is absent in HEK293 cells.[26][27] The monoamine-releasing activities of phenethylamine are abolished in the brain synaptosomes of TAAR1 knockout mice.[111] Conversely however, while TAAR1 may also be involved in the releasing effects of amphetamines, the TAAR1 is not essential for monoamine release induced by amphetamines and other MRAs.[27][23][24][25][26][34]
| Compound | PAL # | 5-HT | NE | DA | Type | Class | Ref |
|---|---|---|---|---|---|---|---|
| 1-Methyl-T | PAL-637 | 53.1 | >10000 | >10000 | SRA | Tryptamine | [11] |
| 1-Phenylpiperazine (PP) | ND | 880 | 186 | 2530 | SNRA | Phenylpiperazine | [86] |
| 2-Aminoindane (2-AI, AI) | ND | >10000 | 86 | 439 | NDRA | Aminoindane | [87] |
| 2-APBT | ND | 8.9 | 21.6 | 38.6 | SNDRA | APBT | [74] |
| 2-BMC | ND | 2837 | 156 | 650 | NDRA | Cathinone | [112] |
| 2-CA | ND | ND | 19.1 | 62.4 | ND | Amphetamine | [4] |
| 2-CMC | ND | 2815 | 93 | 179 | NDRA | Cathinone | [112] |
| 2-FA | ND | ND | 24.1 | 38.1 | ND | Amphetamine | [4] |
| 2-FMA | ND | ~15000 | <100 | ~90 | NDRA | Amphetamine | [113][114] |
| 2-FMC | ND | >10000 | ND (85% at 10 μM) |
48.7 | NDRA | Cathinone | [93] |
| 2-FPM | ND | 4808 | 28 | 112 | NDRA | Phenylmorpholine | [115] |
| 2-MA | ND | ND | 37 | 127 | ND | Amphetamine | [4] |
| 2-MeO-A | ND | ND | 473 | 1478 | ND | Amphetamine | [4] |
| 2-MeO-MC | ND | 7220 | 339 | 920 | NDRA | Cathinone | [112] |
| 2-MMC | ND | 347–490 | 53 | 81–97.9 | SNDRA | Cathinone | [93][112] |
| 2-MPM | ND | 1758 | 102 | 374 | NDRA | Phenylmorpholine | [116] |
| 2-Phenylmorpholine | PAL-632 | 20260 (31% at 10 μM) |
79 (96% at 10 μM) |
86 (98% at 10 μM) |
NDRA | Phenylmorpholine | [117] |
| 2-TFMeO-MC | ND | >10000 | ND (33% at 10 μM) |
>10000 | IA | Cathinone | [93] |
| 2-TFMMC (2-TFMAP) | ND | 8400–>10000 | 2200 (69% at 10 μM) |
8000–>10000 | SNDRA | Cathinone | [118][93][119][112] |
| 2C-C | ND | >100000 | >100000 | 100000 | IA | Phenethylamine | [66][120] |
| 2C-D | ND | IA | IA | IA | IA | Phenethylamine | [120] |
| 2C-E | ND | >100000 | >100000 | >100000 | IA | Phenethylamine | [66][120] |
| 2C-I | ND | >100000 | >100000 | >100000 | IA | Phenethylamine | [66][120] |
| 2C-T-2 | ND | IA | IA | IA | IA | Phenethylamine | [120] |
| 3-APBT | ND | 21.9 | 13.4 | 21.7 | SNDRA | APBT | [74] |
| 3-BCPC | PAL-586 | 621 | ND | IA (RI) | ND | Cathinone | [107] |
| 3-BMC | ND | 136–137 | 25 | 21–28.0 | SNDRA | Cathinone | [93][121][112] |
| 3-CA | PAL-304 | 120 | 9.4 | 11.8 | SNDRA | Amphetamine | [81][4][107][107][122] |
| 3-CC | ND | 567 | 105 | 64 | SNDRA | Cathinone | [123][121] |
| 3-CCPC (RTI-6037-39) | PAL-433 | 1328 | ND | IA (RI) | ND | Cathinone | [107][124] |
| (–)-3-CCPC | PAL-1122 | 562 | ND | IA (RI) | ND | Cathinone | [107] |
| (+)-3-CCPC | PAL-1123 | 733 | ND | IA (RI) | ND | Cathinone | [107] |
| 3-CEC | PAL-361 | IA | ND | IA | ND | Cathinone | [107] |
| 3-Cl-4-Me-CPC | PAL-820 | 181 | ND | IA (RI) | ND | Cathinone | [107] |
| 3′-Cl-5-Me-PM | PAL-738 | 23 | 65 | 58 | SNDRA | Phenylmorpholine | [78][125] |
| 3-CMC (clophedrone) | PAL-434 | 211–410 | 19–54.4 | 26–46.8 | SNDRA | Cathinone | [5][93][121][112][107][126][107] |
| 3-CPC | PAL-363 | IA | ND | IA (RI) | ND | Cathinone | [107] |
| 3′-CPM | PAL-594 | 301 | 75 (82% at 10 μM) |
27 (100% at 10 μM) |
ND | Phenylmorpholine | [125][117] |
| 3-FA | PAL-353 | 1937 | 16.1 | 24.2 | NDRA | Amphetamine | [127][4] |
| 3-FMC | ND | 1460 | ND (100% at 10 μM) |
64.8 | NDRA | Cathinone | [93] |
| 3′-FPM | PAL-593 | 1269–2558 | 17–30 | 43–60 | NDRA | Phenylmorpholine | [115][117] |
| 3-MA | PAL-314 | 218 | 18.3 | 33.3 | NDRA | Amphetamine | [127][81][4] |
| 3-MCPC | PAL-588 | 1067 | ND | IA (RI) | ND | Cathinone | [107] |
| 3-MeO-A | ND | ND | 58.0 | 103 | ND | Amphetamine | [4] |
| 3-MeO-CPC | PAL-591 | 1014 | ND | IA (RI) | ND | Cathinone | [107] |
| 3-MeO-MC | ND | 306–683 | 111 (68% at 10 μM) |
109–129 | SNDRA | Cathinone | [93][121][112] |
| 3-MeO-PM | PAL-823 | ND (78% at 10 μM) |
ND (86% at 10 μM) |
ND (96% at 10 μM) |
ND | Phenylmorpholine | [117] |
| 3-MMC | ND | 268–292 | 27 | 28–70.6 | SNDRA | Cathinone | [5][93][121][112] |
| 3-MPM | PAL-773 | 86 | 62 | 227 | SNDRA | Phenylmorpholine | [116] |
| 3-TFMeO-MC | ND | 188 | ND (79% at 10 μM) |
729 | SNDRA | Cathinone | [93] |
| 3-TFMMC (3-TFMAP) | ND | 297–380 | 2700 (78% at 10 μM) |
610–1290 | SNDRA | Cathinone | [118][93][119][112] |
| 3,4-DCCPC | PAL-787 | 356 | ND | IA (RI) | ND | Cathinone | [107] |
| 4-APBT | ND | 21.2 | 46.2 | 66.6 | SNDRA | APBT | [74] |
| 4-Benzylpiperidine | ND | 5246 | 41.4 | 109 | NDRA | Benzylpiperidine | [128] |
| 4-BMC (brephedrone) | ND | 42.5–60.2 | 100 | 59.4 | SNDRA | Cathinone | [129][93][121][112][130][131] |
| 4-CA (PCA) | ND | 28.3 | 23.5–26.2 | 42.2–68.5 | SNDRA | Amphetamine | [81][4][132][133] |
| 4-CC | ND | 128.4 | 85.1 | 221.8 | SNDRA | Cathinone | [132] |
| 4-CCPC | PAL-743 | 1632 | ND | IA (RI) | ND | Cathinone | [107] |
| 4-CEA (PCEA) | ND | 33.8 | 162.6 | 238.0 | SNDRA | Amphetamine | [132][133] |
| 4-CEC | ND | 152.6 | 5194.0 | 353.6 | SDRA | Cathinone | [132] |
| 4-CMA (PCMA) | ND | 29.9 | 36.5 | 54.7 | SNDRA | Amphetamine | [132][133] |
| 4-CMC (clephedrone) | ND | 71.1–144 | 44–90.9 | 42.2–74.7 | SNDRA | Cathinone | [129][93][132][121][112][130][131] |
| 4-Et-PEA | PAL-505 | ND | ND | 2087 | ND | Phenethylamine | [5] |
| 4-FA | PAL-303 | 730–939 | 28.0–37 | 51.5–200 | NDRA | Amphetamine | [127][66][81][4] |
| 4-Fluoro-T | PAL-551 | 108 | 1123 | 106 | SDRA | Tryptamine | [11] |
| 4-FMC (flephedrone) | ND | 1290–1450 | 62 | 83.4–119 | NDRA | Cathinone | [129][93][121][130][131] |
| 4-FPM | PAL-635 | 2403 (88% at 10 μM) |
285 (100% at 10 μM) |
529 (95% at 10 μM) |
SNDRA | Phenylmorpholine | [117] |
| 4′-FPM | PAL-748 | 1895 | 58 | 191 | NDRA | Phenylmorpholine | [115][117] |
| 4-iPr-PEA | PAL-595 | ND | ND | IA | ND | Phenethylamine | [5] |
| 4-MA | PAL-313 | 53.4 | 22.2 | 44.1 | SNDRA | Amphetamine | [127][81][4] |
| 4-MAR | ND | ND | ND | ND | ND | Phenyloxazolamine | [110] |
| cis-4-MAR | ND | 53.2 | 4.8 | 1.7 | NDRA | Phenyloxazolamine | [110][134] |
| 4-MBA | ND | IA | IA | IA | IA | Amphetamine | [135] |
| 4-MCPC | PAL-744 | 667 | ND | IA (RI) | ND | Cathinone | [107] |
| 4-MEA | ND | 102 | 182 | 550 | SNDRA | Amphetamine | [135] |
| 4-MeO-MC (methedrone) | ND | 120–195 | 111 | 506–881 | SNDRA | Cathinone | [129][93][121][112][130][131] |
| 4-MeO-T | PAL-548 | 4114 | >10000 | >10000 | SRA | Tryptamine | [11] |
| 4-MMA | ND | 67.4 | 66.9 | 41.3 | SNDRA | Amphetamine | [135][130] |
| 4-MPA | ND | 650 | 752 | IA | SNRA | Amphetamine | [135] |
| 4-MPEA (4-Me-PEA) | PAL-503 | ND | ND | 271 | ND | Phenethylamine | [5] |
| 4-MPM | PAL-747 | 86 | 62 | 227 | SNDRA | Phenylmorpholine | [116][117] |
| 4-MTA | ND | ND | ND | ND | SNDRA | Amphetamine | [136][137][138] |
| 4-MTMA | PAL-1063 | 21 | ND | ND | SNDRA | Amphetamine | [78] |
| 4-tBu-MC | ND | IA | ND | 942 (Emax ≈ 50%) |
ND | Cathinone | [139] |
| 4-TFMeO-MC | ND | 118 | ND | 7510 | ND | Cathinone | [93] |
| 4-TFMMC (4-TFMAP) | ND | 190–270 | 900 | 2700–4230 | SNRA | Cathinone | [140][129][118][119][131][112] |
| 4,4'-DMAR | ND | ND | ND | ND | SNDRA | Phenyloxazolamine | ND |
| cis-4,4'-DMAR | ND | 17.7–59.9 | 11.8–31.6 | 8.6–24.4 | SNDRA | Phenyloxazolamine | [134][141][110] |
| trans-4,4'-DMAR | ND | 59.9 | 31.6 | 24.4 | SNDRA | Phenyloxazolamine | [141][110] |
| 5-APB | ND | 19 | 21 | 31 | SNDRA | Amphetamine | [70] |
| 5-APBT | ND | 10.3 | 38.4 | 92.8 | SNDRA | APBT | [74] |
| 5-API (5-IT) | PAL-571 | 28–104.8 | 13.3–79 | 12.9–173 | SNDRA | Amphetamine | [12][76] |
| 5-Bromo-T | PAL-518 | 75.0 | >10000 | 478 | SDRA | Tryptamine | [11] |
| 5-Chloro-αET | PAL-526 | 33.2 | >10000 | IA (RI) | SRA | α-Ethyltryptamine | [11] |
| 5-Chloro-αMT | PAL-542 | 16.2 | 3434 | 54.3 | SDRA | α-Methyltryptamine | [11][12] |
| 5-Chloro-T | PAL-441 | 19.1 | >10000 | 476 | SRA | Tryptamine | [11] |
| 5-Fluoro-αET | PAL-545 | 36.6 | 5334 | 150 | SDRA | α-Ethyltryptamine | [11] |
| 5-Fluoro-αMT | PAL-544 PAL-212 |
14–19 | 78–126 | 32–37 | SNDRA | α-Methyltryptamine | [12][11][42] |
| 5-Fluoro-T | PAL-284 | 10.1 | 464 | 82.3 | SDRA | Tryptamine | [11] |
| 5-MABB (5-MBPB) | ND | ND | ND | ND | ND | Amphetamine | [73][142] |
| (S)-5-MABB | ND | 31 | 158 | 210 | SNDRA | Amphetamine | [73][142] |
| (R)-5-MABB | ND | 49 | 850 | IA | SRA | Amphetamine | [73][142] |
| 5-MAPB | ND | 64–90 | 24 | 41–459 | SNDRA | Amphetamine | [70][143] |
| (S)-5-MAPB | ND | 67 | ND | 258 | ND | Amphetamine | [143] |
| (R)-5-MAPB | ND | 184 | ND | 1951 | ND | Amphetamine | [143] |
| 5-MeO-αMT | ND | 460 | 8900 | 1500 | SNDRA | α-Methyltryptamine | [66] |
| 5-MeO-DALT | ND | >100000 | >100000 | >100000 | IA | Tryptamine | [66] |
| 5-MeO-DET | ND | IA (RI) | IA | IA | SRI | Tryptamine | [42] |
| 5-MeO-DiPT | ND | >100000 (RI) | >100000 (RI) | >100000 | IA | Tryptamine | [66][42] |
| 5-MeO-DMT | ND | >100000 (RI) | >100000 (RI) | >100000 | IA | Tryptamine | [66][42] |
| 5-MeO-DPT | ND | IA (RI) | IA | IA (RI) | SRI | Tryptamine | [42] |
| 5-MeO-MiPT | ND | >100000 | >100000 | >100000 | IA | Tryptamine | [66][42] |
| 5-MeO-NET | ND | 284 | >10000 | >10000 | SRA | Tryptamine | [42] |
| 5-MeO-NiPT | ND | IA (RI) | IA | IA | SRI | Tryptamine | [42] |
| 5-MeO-NMT | ND | 1114 | >10000 | >10000 | SRA | Tryptamine | [42] |
| 5-MeO-T | PAL-234 | 2169 | >10000 | 11031 | SDRA | Tryptamine | [11][42] |
| 5-Methyl-T | PAL-22 | 139 | >10000 | >10000 | SRA | Tryptamine | [11] |
| 6-APB | ND | 36 | 14 | 10 | SNDRA | Amphetamine | [70] |
| 6-APBT | ND | 10.7 | 13.6 | 7.2 | SNDRA | APBT | [74] |
| 6-API (6-IT) | ND | 19.9 | 25.6 | 164.0 | SNDRA | Amphetamine | [76] |
| 6-Fluoro-T | PAL-227 | 4.4 | 1575 | 106 | SRA | Tryptamine | [11] |
| 6-MABB (6-MBPB) | ND | ND | ND | ND | ND | Amphetamine | [73][142] |
| (R)-6-MABB | ND | 172 | 227 | IA | SNRA | Amphetamine | [73][142] |
| (S)-6-MABB | ND | 54 | 77 | 41 | SNDRA | Amphetamine | [73][142] |
| 6-MAPB | ND | 33 | 14 | 20 | SNDRA | Amphetamine | [70] |
| 6-MeO-T | PAL-263 | 53.8 | 465 | 113 | SNDRA | Tryptamine | [11] |
| 6-Methyl-T | PAL-522 | 51.6 | >10000 | 353 | SDRA | Tryptamine | [11] |
| 7-APBT | ND | 36.9 | 28.5 | 16.8 | SNDRA | APBT | [74] |
| 7-Chloro-T | PAL-532 | 8.03 | 656 | 1330 | SRA | Tryptamine | [11] |
| 7-MeO-T | PAL-533 | 44.6 | 5600 | 2118 | SRA | Tryptamine | [11] |
| 7-Methyl-T | PAL-286 | 23.7 | >10000 | 3380 | SRA | Tryptamine | [11] |
| α-Ethyltryptamine (AET, αET) | PAL-125 | 23.2 | 640 | 232 | SDRA | α-Ethyltryptamine | [11] |
| (–)-α-Ethyltryptamine | PAL-640 | 54.9 | 3670 | 654 | SRA | α-Ethyltryptamine | [11] |
| (+)-α-Ethyltryptamine | PAL-647 | 34.7 | 592 | 57.6 | SDRA | α-Ethyltryptamine | [11] |
| α-Me-MC (βk-mephentermine; RAD-081) | ND | 12860 | 153 | 590 | NDRA | Cathinone | [144][145][146] |
| α-Methylisotryptamine (isoAMT) | PAL-569 | 177 | 81 | 1062 | SNRA | Isotryptamine | [12] |
| α-Methyltryptamine (αMT; AMT) | PAL-17 | 21.7–68 | 79–112 | 78.6–180 | SNDRA | α-Methyltryptamine | [66][11][147] |
| βk-NMPEA (FTS-096) | ND | >60000 | 148 | 1860 | NRA | Phenethylamine | [144][145][146] |
| AMAPN | ND | 21 | ND | 55 | ND | Cathinone | [93][148] |
| Amfepramone (diethylpropion) | ND | >10000 | >10000 | >10000 | PD | Cathinone | [149][106] |
| Aminorex | ND | 193–414 | 15.1–26.4 | 9.1–49.4 | SNDRA | Phenyloxazolamine | [41][134][4][110][106] |
| Amphetamine (A) | ND | ND | ND | ND | NDRA | Amphetamine | ND |
| Dextroamphetamine | ND | 698–1765 | 6.6–10.2 | 5.8–24.8 | NDRA | Amphetamine | [41][150][4][139][106] |
| Levoamphetamine | ND | ND | 9.5 | 27.7 | NDRA | Amphetamine | [81][4][151][152] |
| APPEA (α-Pr-PEA) | PAL-550 | IA | ND | IA (RI) | ND | Amphetamine | [5][107] |
| BDB | ND | 180 | 540 | 2,300 | NDRA | Amphetamine | [66] |
| Benzylpiperazine (BZP) | ND | 6050–>10000 | 62–68 | 175–600 | NDRA | Phenylpiperazine | [66][153][3][4][154] |
| BK-NM-AMT | ND | 41.3 | ND (55% at 10 μM) |
92.8 | SDRA | α-Methyltryptamine | [93][148][94] |
| BK-5F-NM-AMT | ND | 190 | ND | 620 | ND | α-Methyltryptamine | [155] |
| BK-5Cl-NM-AMT | ND | 200 | ND | 865 | ND | α-Methyltryptamine | [155] |
| BK-5Br-NM-AMT | ND | 295 | ND | 2100 | ND | α-Methyltryptamine | [155] |
| BMAPN | ND | 27 | ND | 34 | ND | Cathinone | [93][148] |
| BMPEA (β-Me-PEA) | ND | ND | 126 | 627 | ND | Phenethylamine | [156] |
| Bufotenin (DMS, 5-HO-DMT) | ND | 30.5 | >10000 | >10000 | SRA | Tryptamine | [42] |
| Buphedrone (βk-MEPEA) | PAL-429 | IA | ND | 411 | ND | Cathinone | [107] |
| Bupropion (amfebutamone) | ND | IA (RI) | IA (RI) | IA (RI) | NDRI | Cathinone | [146][123][121] |
| Butylamphetamine (NBA, BA) | PAL-90 | ND | ND | IA | ND | Amphetamine | [5] |
| Butylone (βk-MBDB) | ND | 330 | IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [157][158] |
| Cathinone (C; βk-AMPH) | ND | 6100–7595 | 23.6–25.6 | 34.8–83.1 | NDRA | Cathinone | [4][93][132] |
| D-Cathinone | ND | >10000 | 72.0 | 183.9 | NDRA | Cathinone | [159] |
| L-Cathinone | ND | 2366–9267 | 12.4–28 | 18–24.6 | NDRA | Cathinone | [160][123][159] |
| Chlorphentermine | ND | 18.2–30.9 | >10000 (RI) | 935–2650 | SRA | Amphetamine | [41][106] |
| DEPEA (α-Et-EPEA) | ND | ND | 209 | 604 | ND | Amphetamine | [161] |
| Dibutylone | ND | IA | IA (RI) | IA (RI) | DRI | Cathinone | [162] |
| Diethyltryptamine (DET) | ND | IA (RI) | IA | IA | SRI | Tryptamine | [42] |
| Diisopropyltryptamine (DiPT) | ND | IA (RI) | IA (RI) | IA | SRI | Tryptamine | [42] |
| Dimethylamphetamine | ND | ND | 223 | 1250 | ND | Amphetamine | [156] |
| Dimethyltryptamine (DMT) | ND | 114 | 4166 | >10000 | SRA | Tryptamine | [42] |
| Dipropyltryptamine (DPT) | ND | >100000 (RI) | >100000 (RI) | >100000 (RI) | IA | Tryptamine | [66][42] |
| DMPP (2,3-DMPP) | PAL-218 | 24–26 | 13.7–56 | 1207–1320 | SNRA | Phenylpiperazine | [78][86] |
| DOC | ND | IA | IA | IA | IA | Amphetamine | [120] |
| Dopamine (DA) | ND | >10000 (RI) | 66.2 | 86.9 | NDRA | Phenethylamine | [41][4] |
| EDMA | ND | 117 | 325 | 597 | SNDRA | Amphetamine | [67][130] |
| EDMC | ND | 347 | 327 | 496 | SNDRA | Cathinone | [67][130] |
| ENAP | PAL-1045 | 12 | 137 | 46 | SDRA | Amphetamine | [78] |
| Ephedrine (racephedrine) | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Ephedrine (ephedrine) | ND | >10000 | 43.1–72.4 | 236–1350 | NDRA | Cathinol | [41][4] |
| L-Ephedrine | ND | >10000 | 218 | 2104 | NRA | Cathinol | [41][160] |
| Ephylone | ND | IA (RI) | IA (RI) | IA (RI) | IA (NDRI) | Cathinone | [163] |
| Epinephrine | ND | ND | ND | ND | NDRA | Phenethylamine | ND |
| Ethcathinone (EC) | ND | 1923–2118 | 88.3–99.3 | 267.6–>1000 | NRA | Cathinone | [149][4][132][139] |
| Ethylamphetamine (EA) | PAL-99 | ND | ND | 88.5 | ND | Amphetamine | [5] |
| S(+)-Ethylamphetamine | ND | 333.0 | 28.8 | 44.1 | NDRA | Amphetamine | [132][133] |
| Ethylone (βk-MDEA) | ND | 617.4 | 4251 | 1122 | SNDRA | Cathinone | [130] |
| Eutylone (βk-EBDB) | ND | 1020 | IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [162] |
| Fenfluramine (3-TFM-EA) | ND | 79.3–108 | 739 | >10000 (RI) | SRA | Amphetamine | [41][164][165][4] |
| D-Fenfluramine | ND | 51.7 | 302 | >10000 | SNRA | Amphetamine | [41][164] |
| L-Fenfluramine | ND | 147 | >10000 | >10000 | SRA | Amphetamine | [164][166] |
| HHA | ND | ND | 33 | 3485 | ND | Amphetamine | [4] |
| HHMA | ND | 1729 | 77 | 130 | NDRA | Amphetamine | [4][167] |
| HHMC | ND | 14100 | 110 | 90 | NDRA | Cathinone | [168] |
| HMA | ND | 897 | 694 | 1450–3423 | SNDRA | Amphetamine | [4][169][170] |
| HMMA | ND | 589–607 | 625 | 607–3652 | SNDRA | Amphetamine | [4][169][170][167] |
| HMMC | ND | 7210 | 6340 | 5840 | SNDRA | Cathinone | [168] |
| MBDB | ND | 540 | 3300 | >100000 | SNRA | Amphetamine | [66] |
| mCPP (3-CPP, 3CPP) | ND | 28–38.1 | ≥1400 | 63000 | SRA | Phenylpiperazine | [66][166][171] |
| MDA | ND | 160–162 | 47–108 | 106–190 | SNDRA | Amphetamine | [165][4][70] |
| (R)-MDA | ND | 310 | 290 | 900 | SNDRA | Amphetamine | [165][4] |
| (S)-MDA | ND | 100 | 50.0 | 98.5 | SNDRA | Amphetamine | [165][4] |
| MDAI | ND | 114 | 117 | 1334 | SNRA | Aminoindane | [87] |
| MDC | ND | 966 | 394 | 370 | SNDRA | Cathinone | [168] |
| MDEA | PAL-192 | 47 | 2608 | 622 | SNDRA | Amphetamine | [78] |
| (R)-MDEA | PAL-193 | 52 | 651 | 507 | SNDRA | Amphetamine | [78] |
| (S)-MDEA | PAL-194 | 465 | RI | RI | SRA | Amphetamine | [78] |
| MDMA | ND | 50–85 | 54–110 | 51–278 | SNDRA | Amphetamine | [41][172][76][165][4][70] |
| (R)-MDMA | ND | 340 | 560 | 3700 | SNDRA | Amphetamine | [165][4] |
| (S)-MDMA | ND | 74 | 136 | 142 | SNDRA | Amphetamine | [165][4] |
| MDMAR | ND | ND | ND | ND | SNDRA | Phenyloxazolamine | ND |
| cis-MDMAR | ND | 43.9 | 14.8 | 10.2 | SNDRA | Phenyloxazolamine | [141] |
| trans-MDMAR | ND | 73.4 | 38.9 | 36.2 | SNDRA | Phenyloxazolamine | [141] |
| MDPV | ND | IA | 13 (Emax = 24%) |
2.3 (Emax = 24%) |
NDRI | Phenylethylpyrrolidine | [150][130] |
| MEAI (5-MeO-AI) | ND | 134 | 861 | 2646 | SNRA | Aminoindane | [87] |
| MEPEA (α-Et-MPEA) | PAL-426 | 4698 | 58 | 179–225 | SNDRA | Amphetamine | [107][161] |
| Mephedrone (4-MMC) | ND | 118.3–122 | 58–62.7 | 49.1–51 | SNDRA | Cathinone | [172][150][93][112][131] |
| S(–)-Mephedrone | ND | 61 | ND | 74 | ND | Cathinone | [139][173] |
| R(+)-Mephedrone | ND | 1470 | ND | 31 | ND | Cathinone | [139][173] |
| Mesocarb | ND | ND | ND | >100000 (RI) | DRI | Amphetamine | [174] |
| Methamphetamine (MA) | ND | ND | ND | ND | NDRA | Amphetamine | ND |
| Dextromethamphetamine | ND | 736–1292 | 12.3–14.3 | 8.5–40.4 | NDRA | Amphetamine | [41][172][4][106] |
| Levomethamphetamine | ND | 4640 | 28.5 | 416 | NRA | Amphetamine | [41][4] |
| Methcathinone (MC) | ND | 2592–5853 | 22–26.1 | 12.5–49.9 | NDRA | Cathinone | [4][93][121][112][132] |
| D-Methcathinone | ND | IA | ND | ND | NRA | Cathinone | [146] |
| L-Methcathinone | ND | 1772 | 13.1 | 14.8 | NDRA | Cathinone | [160][139] |
| Methiopropamine | ND | IA (RI) | IA (RI) | IA (RI) | NDRI | Thiopropamine | [175][176] |
| Methylone (MDMC) | ND | 234–708 | 140–270 | 117–220 | SNDRA | Cathinone | [172][150][130][162][168] |
| Methylphenidate | ND | IA (RI) | IA (RI) | IA (RI) | NDRI | Phenidate | [3][52][177] |
| Mexedrone (4-MMC-MeO) | ND | 2525 | IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [178] |
| MiPT | ND | IA | IA | IA | IA | Tryptamine | [42] |
| MMAI | ND | 31 | 3101 | >10000 | SRA | Aminoindane | [87] |
| MNAP (methamnetamine) | PAL-1046 | 13 | 34 | 10 | SNDRA | Amphetamine | [78][5] |
| MPPA (BMMPEA, β-Me-NMPEA) | ND | ND | 154 | 574 | ND | Phenethylamine | [156] |
| Naphthylisopropylamine (NAP) | PAL-287 | 3.4 | 11.1 | 12.6 | SNDRA | Amphetamine | [179][4] |
| Naphthylmetrazine | PAL-704 | IA (RI | 203 | 111 | NDRA/SRI | Phenylmorpholine | [117] |
| Naphthylmorpholine | PAL-678 | ND (92% at 10 μM) |
ND (88% at 10 μM) |
ND (79% at 10 μM) |
ND | Phenylmorpholine | [117] |
| NET (NETP; N-Et-T) | PAL-536 | 18.6 | IA (RI) | IA (RI) | SRA | Tryptamine | [11][42] |
| NiPT | ND | IA (RI) | IA | IA | SRI | Tryptamine | [42] |
| NMT | PAL-152 | 22.4 | 733 | 321 | SRA | Tryptamine | [11][42] |
| Norephedrine (phenylpropanolamine) | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Norephedrine | ND | >10000 | 42.1 | 302 | NDRA | Cathinol | [160] |
| L-Norephedrine | ND | >10000 | 137 | 1371 | NRA | Cathinol | [160] |
| Norepinephrine (NE) | ND | >10000 | 164 | 869 | NDRA | Phenethylamine | [41][4] |
| Norfenfluramine (3-TFMA) | ND | 104 | 168–170 | 1900–1925 | SNRA | Amphetamine | [164][165] |
| (+)-Norfenfluramine | ND | 59.3 | 72.7 | 924 | SNRA | Amphetamine | [164] |
| (–)-Norfenfluramine | ND | 287 | 474 | >10000 | SNRA | Amphetamine | [164] |
| Normephedrone (4-MC) | ND | 210 | 100 | 220 | SNDRA | Cathinone | [180][159][139] |
| R(+)-Normephedrone | ND | 179 | 89 | 150 | SNDRA | Cathinone | [139][159] |
| S(–)-Normephedrone | ND | 1592 | 115 | 391 | NDRA | Cathinone | [139][159] |
| Norpropylhexedrine | ND | ND | ND | ND | NDRA | Cyclohexylethylamine | ND |
| Norpseudoephedrine | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Norpseudoephedrine (cathine) | ND | >10000 | 15.0 | 68.3 | NDRA | Cathinol | [160] |
| L-Norpseudoephedrine | ND | >10000 | 30.1 | 294 | NDRA | Cathinol | [160] |
| ODMA | ND | ND | ND | ND | SNDRA | Amphetamine | [80] |
| oMPP (2-MPP) | PAL-169 | 175 | 39.1 | 296–542 | SNDRA | Phenylpiperazine | [181][5][86] |
| PMA (4-MeO-A) | ND | ND | 166 | 867 | SNDRA | Amphetamine | [4][92][138] |
| PMMA (4-MeO-MA) | ND | ND | ND | ND | SNDRA | Amphetamine | [138] |
| (S)-PMMA | ND | 41 | 147 | 1000 | SNRA | Amphetamine | [140][182][92] |
| (R)-PMMA | ND | 134 | >14000 | 1600 | SRA | Amphetamine | [140][182][92] |
| Pentylone | ND | 476–1030 (Emax ≈ 50%) |
IA (RI) | IA (RI) | SRA/NDRI | Cathinone | [157][162][163] |
| Phenacylamine (βk-PEA) | PAL-27 | >10000 | ND (96% at 10 μM) |
208 | NDRA | Phenethylamine | [5][93][139] |
| Phendimetrazine | ND | >100000 | >10000 | >10000 | PD | Phenylmorpholine | [183][4][106] |
| Phenethylamine (PEA) | ND | >10000 | 10.9 | 39.5 | NDRA | Phenethylamine | [5][81][4] |
| Phenmetrazine (PM) | PAL-55 | 7765–>10000 | 29–50.4 | 70–131 | NDRA | Phenylmorpholine | [183][4][116][117] |
| Phentermine (P, PH) | ND | 2575–3511 | 28.8–39.4 | 262 | NDRA | Amphetamine | [41][4][106] |
| Phenylalaninol | ND | ND | ND | ND | ND | Amphetamine | ND |
| D-Phenylalaninol | PAL-329 | >10000 | 106 | 1355 | NRA | Amphetamine | [181] |
| Phenylbutenamine | ND | ND | ND | ND | ND | Phenylbutenamine | ND |
| (3E)-Phenylbutenamine | PAL-881 | >10000 | 308 | 666 | SNRA | Phenylbutenamine | [82][83] |
| (3Z)-Phenylbutenamine | PAL-893 | >10000 | 301 | 1114 | SNRA | Phenylbutenamine | [82][83] |
| Phenylbutynamine | PAL-874 | >10000 | 305 | 688 | NDRA | Phenylbutynamine | [78] |
| Phenylisobutylamine (α-Et-PEA, AEPEA) | PAL-426 | 4698 | 80 | 225–273 | NDRA | Amphetamine | [5][107][122][161] |
| Phenylpropylamine | ND | ND | 222 | 1491 | NDRA | Phenylpropylamine | [81][4] |
| pMeOPP (4-MeOPP) | ND | 3200 | 440–1500 | 6300–11000 | SNRA | Phenylpiperazine | [66][86] |
| pMPP (4-MPP) | PAL-233 | ND | ND | IA (RI) | ND | Phenylpiperazine | [5] |
| pNPP (4-NPP) | PAL-175 | 19–43 (Emax = 57%) |
>10000 | >10000 | SRA | Phenylpiperazine | [78][86] |
| Propylamphetamine (PA) | PAL-424 | ND | ND | RI (1013) | ND | Amphetamine | [5] |
| Propylcathinone (PC) | PAL-359 | ND | ND | IA | ND | Cathinone | [5][139] |
| Propylhexedrine | ND | ND | ND | ND | NDRA | Cyclohexylethylamine | ND |
| Propylone | ND | 3128 | IA (RI) | 975.9 | SDRA | Cathinone | [130] |
| Pseudoephedrine (racemic) | ND | ND | ND | ND | NDRA | Cathinol | ND |
| D-Pseudoephedrine | ND | >10000 | 4092 | 9125 | NDRA | Cathinol | [160] |
| L-Pseudoephedrine (pseudoephedrine) | ND | >10000 | 224 | 1988 | NRA | Cathinol | [160] |
| Pseudophenmetrazine | ND | >10000 | 514 | RI | NRA | Phenylmorpholine | [183] |
| Psilocin | PAL-153 | 561 (Emax = 54%) |
>10000 | >10000 | SRA | Tryptamine | [78][42] |
| SeDMA | ND | ND | ND | ND | SNDRA | Amphetamine | [80] |
| Serotonin (5-HT) | ND | 44.4 | >10000 (RI) | ≥1960 | SRA | Tryptamine | [41][4] |
| TDMA | ND | ND | ND | ND | SNDRA | Amphetamine | [80] |
| TFMCPP (3-TFM-4-C-PP) | PAL-179 | 33 (Emax = 66%) |
>10000 | >10000 | SRA | Phenylpiperazine | [78] |
| TFMPP (3-TFMPP) | ND | 121 | >10000 | >10000 | SRA | Phenylpiperazine | [153][154][4] |
| TMA (3,4,5-TMeO-A) | ND | 16000 | >100000 | >100000 | IA | Amphetamine | [66] |
| TMA-2 (2,4,5-TMeO-A) | ND | >100000 | >100000 | >100000 | IA | Amphetamine | [66] |
| TMA-6 (2,4,6-TMeO-A) | ND | >100000 | >100000 | >100000 | IA | Amphetamine | [66] |
| Tramadol | ND | IA (RI) | IA (RI) | IA | SNRI | ND | [3] |
| Tryptamine (T) | PAL-235 | 32.6 | 716 | 164 | SDRA | Tryptamine | [42][11] |
| Tyramine | ND | 2775 | 40.6 | 119 | NDRA | Phenethylamine | [41][4] |
| Notes: (1) The smaller the value, the more potently the substance releases the neurotransmitter. (2) These values were from assays conducted using rat brain synaptosomes. Values from other methods of quantifying monoamine release, such as HEK293 cells transfected with monoamine transporters, are not fully analogous to neuronal cells and result in much different and lower potencies. As a result, they are not included in this table. | |||||||
References
[edit]- ^ a b c d e f Heal DJ, Smith SL, Gosden J, Nutt DJ (June 2013). "Amphetamine, past and present--a pharmacological and clinical perspective". Journal of Psychopharmacology. 27 (6): 479–496. doi:10.1177/0269881113482532. PMC 3666194. PMID 23539642.
- ^ a b c d e f g h i j k Rothman RB, Baumann MH (October 2003). "Monoamine transporters and psychostimulant drugs". European Journal of Pharmacology. 479 (1–3): 23–40. doi:10.1016/j.ejphar.2003.08.054. PMID 14612135.
- ^ a b c d e f g h i j k l m n o Rothman RB, Baumann MH (2006). "Therapeutic potential of monoamine transporter substrates". Current Topics in Medicinal Chemistry. 6 (17): 1845–1859. doi:10.2174/156802606778249766. PMID 17017961.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be Blough B (July 2008). "Dopamine-releasing agents" (PDF). In Trudell ML, Izenwasser S (eds.). Dopamine Transporters: Chemistry, Biology and Pharmacology. Hoboken [NJ]: Wiley. pp. 305–320. ISBN 978-0-470-11790-3. OCLC 181862653. OL 18589888W.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am Reith ME, Blough BE, Hong WC, Jones KT, Schmitt KC, Baumann MH, et al. (February 2015). "Behavioral, biological, and chemical perspectives on atypical agents targeting the dopamine transporter". Drug and Alcohol Dependence. 147: 1–19. doi:10.1016/j.drugalcdep.2014.12.005. PMC 4297708. PMID 25548026.
Converging lines of evidence have solidified the notion that DA releasers are substrates of the transporter and once translocated, they reverse the normal direction of transporter flux to evoke release of endogenous neurotransmitters. The nature of this reversal is not well understood, but the entire process is primarily transporter-dependent and requires elevated intracellular sodium concentrations, phosphorylation of DAT, and possible involvement of transporter oligomers (Khoshbouei et al., 2003, 2004; Sitte and Freissmuth, 2010). [...] Generic pharmacophore for biogenic amine transporter ligands. Note that transportable substrate ligands exhibit size constraints defined by the red circle. Functional groups attached to the nitrogen, α-carbon or phenyl ring that extend beyond the "edge" of the pharmacophore will generate partial substrates, transporter blockers or be inactive.
- ^ a b c d Schmitt KC, Rothman RB, Reith ME (July 2013). "Nonclassical pharmacology of the dopamine transporter: atypical inhibitors, allosteric modulators, and partial substrates". The Journal of Pharmacology and Experimental Therapeutics. 346 (1): 2–10. doi:10.1124/jpet.111.191056. PMC 3684841. PMID 23568856.
- ^ a b c d e f Heal DJ, Gosden J, Smith SL (December 2014). "Dopamine reuptake transporter (DAT) "inverse agonism"--a novel hypothesis to explain the enigmatic pharmacology of cocaine". Neuropharmacology. 87: 19–40. doi:10.1016/j.neuropharm.2014.06.012. PMID 24953830.
- ^ a b c d e Shimazu S, Miklya I (May 2004). "Pharmacological studies with endogenous enhancer substances: beta-phenylethylamine, tryptamine, and their synthetic derivatives". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 28 (3): 421–427. doi:10.1016/j.pnpbp.2003.11.016. PMID 15093948. S2CID 37564231.
- ^ a b c d e Knoll J (August 2003). "Enhancer regulation/endogenous and synthetic enhancer compounds: a neurochemical concept of the innate and acquired drives". Neurochemical Research. 28 (8): 1275–1297. doi:10.1023/a:1024224311289. PMID 12834268.
- ^ Rothman RB, Blough BE, Baumann MH (January 2007). "Dual dopamine/serotonin releasers as potential medications for stimulant and alcohol addictions". The AAPS Journal. 9 (1): E1-10. doi:10.1208/aapsj0901001. PMC 2751297. PMID 17408232.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae Blough BE, Landavazo A, Partilla JS, Decker AM, Page KM, Baumann MH, et al. (October 2014). "Alpha-ethyltryptamines as dual dopamine-serotonin releasers". Bioorganic & Medicinal Chemistry Letters. 24 (19): 4754–4758. doi:10.1016/j.bmcl.2014.07.062. PMC 4211607. PMID 25193229.
- ^ a b c d e f g Banks ML, Bauer CT, Blough BE, Rothman RB, Partilla JS, Baumann MH, et al. (June 2014). "Abuse-related effects of dual dopamine/serotonin releasers with varying potency to release norepinephrine in male rats and rhesus monkeys". Experimental and Clinical Psychopharmacology. 22 (3): 274–284. doi:10.1037/a0036595. PMC 4067459. PMID 24796848.
- ^ Brust JC (2004). Neurological Aspects of Substance Abuse. Butterworth-Heinemann. pp. 117–. ISBN 978-0-7506-7313-6.
- ^ Competitive problems in the drug industry: hearings before Subcommittee on Monopoly and Anticompetitive Activities of the Select Committee on Small Business, United States Senate, Ninetieth Congress, first session. U.S. Government Printing Office. 1976. pp. 2–.
- ^ Parrott AC, Stuart M (1 September 1997). "Ecstasy (MDMA), amphetamine, and LSD: comparative mood profiles in recreational polydrug users". Human Psychopharmacology: Clinical and Experimental. 12 (5): 501–504. CiteSeerX 10.1.1.515.2896. doi:10.1002/(sici)1099-1077(199709/10)12:5<501::aid-hup913>3.3.co;2-m. ISSN 1099-1077.
- ^ Scorza C, Silveira R, Nichols DE, Reyes-Parada M (July 1999). "Effects of 5-HT-releasing agents on the extracellullar hippocampal 5-HT of rats. Implications for the development of novel antidepressants with a short onset of action". Neuropharmacology. 38 (7): 1055–1061. doi:10.1016/s0028-3908(99)00023-4. PMID 10428424.
- ^ Morean ME, de Wit H, King AC, Sofuoglu M, Rueger SY, O'Malley SS (May 2013). "The drug effects questionnaire: psychometric support across three drug types". Psychopharmacology. 227 (1): 177–192. doi:10.1007/s00213-012-2954-z. PMC 3624068. PMID 23271193.
- ^ Nelson RA, Boyd SJ, Ziegelstein RC, Herning R, Cadet JL, Henningfield JE, et al. (March 2006). "Effect of rate of administration on subjective and physiological effects of intravenous cocaine in humans". Drug and Alcohol Dependence. 82 (1): 19–24. doi:10.1016/j.drugalcdep.2005.08.004. PMID 16144747.
- ^ Berlin I, Warot D, Aymard G, Acquaviva E, Legrand M, Labarthe B, et al. (September 2001). "Pharmacodynamics and pharmacokinetics of single nasal (5 mg and 10 mg) and oral (50 mg) doses of ephedrine in healthy subjects". European Journal of Clinical Pharmacology. 57 (6–7): 447–455. doi:10.1007/s002280100317. PMID 11699608. S2CID 12410591.
- ^ Powers ME (October 2001). "Ephedra and its application to sport performance: another concern for the athletic trainer?". Journal of Athletic Training. 36 (4): 420–424. PMC 155439. PMID 16558668.
- ^ Meeusen R, Watson P, Hasegawa H, Roelands B, Piacentini MF (1 January 2006). "Central fatigue: the serotonin hypothesis and beyond". Sports Medicine. 36 (10): 881–909. doi:10.2165/00007256-200636100-00006. PMID 17004850. S2CID 5178189.
- ^ Roelands B, Meeusen R (March 2010). "Alterations in central fatigue by pharmacological manipulations of neurotransmitters in normal and high ambient temperature". Sports Medicine. 40 (3): 229–246. doi:10.2165/11533670-000000000-00000. PMID 20199121. S2CID 25717280.
- ^ a b c d e Miller GM (January 2011). "The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity". Journal of Neurochemistry. 116 (2): 164–176. doi:10.1111/j.1471-4159.2010.07109.x. PMC 3005101. PMID 21073468.
- ^ a b Wu R, Liu J, Li JX (2022). "Trace amine-associated receptor 1 and drug abuse". Behavioral Pharmacology of Drug Abuse: Current Status. Adv Pharmacol. Vol. 93. pp. 373–401. doi:10.1016/bs.apha.2021.10.005. ISBN 978-0-323-91526-7. PMC 9826737. PMID 35341572.
It is reported that methamphetamine (METH) interacts with TAAR1 and subsequently inhibits DA uptake, enhance DA efflux and induces DAT internalization, and these effects are dependent on TAAR1 (Xie & Miller, 2009). For example, METH-induced inhibition of DA uptake was observed in TAAR1 and DAT cotransfected cells and WT mouse and monkey striatal synaptosomes but not in DAT-only transfected cells or in striatal synaptosomes of TAAR1-KO mice (Xie & Miller, 2009). TAAR1 activation was enhanced by co-expression of monoamine transporters and this effect could be blocked by monoamine transporter antagonists (Xie & Miller, 2007; Xie et al., 2007). Furthermore, DA activation of TAAR1 induced C-FOS-luciferase expression only in the presence of DAT (Xie et al., 2007).
- ^ a b Xie Z, Miller GM (July 2009). "A receptor mechanism for methamphetamine action in dopamine transporter regulation in brain". The Journal of Pharmacology and Experimental Therapeutics. 330 (1): 316–325. doi:10.1124/jpet.109.153775. PMC 2700171. PMID 19364908.
- ^ a b c d e Lewin AH, Miller GM, Gilmour B (December 2011). "Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class". Bioorganic & Medicinal Chemistry. 19 (23): 7044–7048. doi:10.1016/j.bmc.2011.10.007. PMC 3236098. PMID 22037049.
While our data suggest a role for TAAR1 in eliciting amphetamine-like stimulant effects, it must be borne in mind that the observed in vivo effects are likely to result from interaction with both TAAR1 and monoamine transporters. Thus it has been shown that the selective TAAR1 agonist RO5166017 fully prevented psychostimulant-induced and persistent hyperdopaminergia-related hyperactivity in mice.42 This effect was found to be DAT-independent, since suppression of hyperactivity was observed in DAT-KO mice.42 The collected information leads us to conclude that TAAR1 is a stereoselective binding site for amphetamine and that TAAR1 activation by amphetamine and its congeners may contribute to the stimulant properties of this class of compounds. [...] it has been shown that β-PEA and methamphetamine effects in cells expressing TAAR-DAT significantly exceed those observed in cells expressing DAT only. Consistent with this conclusion is the higher potency of (S)-[amphetamine] in rat synaptosomes relative to cloned human DAT cells (EC50 60 nM vs 240 nM).
- ^ a b c d e f g h Small C, Cheng MH, Belay SS, Bulloch SL, Zimmerman B, Sorkin A, et al. (August 2023). "The Alkylamine Stimulant 1,3-Dimethylamylamine Exhibits Substrate-Like Regulation of Dopamine Transporter Function and Localization". J Pharmacol Exp Ther. 386 (2): 266–273. doi:10.1124/jpet.122.001573. PMC 10353075. PMID 37348963.
[...] a proposed intracellular target for amphetamine is the [TAAR1], a [GPCR] that is expressed on intracellular membranes in DA neurons (Miller, 2011). Phenethylamine stimulants have been proposed to activate TAAR1, leading to increased cAMP generation and RhoA activation, with subsequent enhancement of DAT reverse transport and endocytosis (Xie and Miller, 2007, 2008, 2009; Underhill et al., 2021). Methamphetamine-induced DAT endocytosis was found to be dependent on TAAR1 expression and PKA activity as suggested by use of the kinase inhibitor H89 (Xie and Miller, 2009). However, evidence indicating that amphetamine-induced endocytosis is independent of TAAR1 includes 1) HEK-293 cells do not express TAAR1 (Reese et al., 2007; Xie and Miller, 2007) but do exhibit amphetamine-induced DAT endocytosis [present studies and (Saunders et al., 2014; Cheng et al., 2015; Wheeler et al., 2015)]; 2) cAMP and PKA activation, which are stimulated by TAAR1, antagonized amphetamine-induced DAT endocytosis in heterologous cells and DA neurons [present studies and (Wheeler et al., 2015)]; and 3) in cell lines and rodent striatal synaptosomes, PKA activation increased DAT Vmax, consistent with increased plasma membrane expression (Pristupa et al., 1998; Page et al., 2004; Batchelor and Schenk, 2018). Additionally, DMAA induced DAT endocytosis (Figs. 3 and 4) despite exhibiting no activity at human TAAR1 in receptor binding studies (Rickli et al., 2019). Therefore, although some evidence does support a role of TAAR1 in modulating amphetamine-induced DAT endocytosis, the present studies suggest that DMAA and amphetamine promote DAT endocytosis through a TAAR1-independent mechanism.
- ^ a b Espinoza S, Gainetdinov RR (2014). "Neuronal Functions and Emerging Pharmacology of TAAR1". Taste and Smell. Topics in Medicinal Chemistry. Vol. 23. Cham: Springer International Publishing. pp. 175–194. doi:10.1007/7355_2014_78. ISBN 978-3-319-48925-4.
- ^ a b Liu J, Wu R, Li JX (March 2020). "TAAR1 and Psychostimulant Addiction". Cellular and Molecular Neurobiology. 40 (2): 229–238. doi:10.1007/s10571-020-00792-8. PMC 7845786. PMID 31974906.
- ^ a b Lindemann L, Meyer CA, Jeanneau K, Bradaia A, Ozmen L, Bluethmann H, et al. (March 2008). "Trace amine-associated receptor 1 modulates dopaminergic activity". The Journal of Pharmacology and Experimental Therapeutics. 324 (3): 948–956. doi:10.1124/jpet.107.132647. PMID 18083911.
- ^ a b Achat-Mendes C, Lynch LJ, Sullivan KA, Vallender EJ, Miller GM (April 2012). "Augmentation of methamphetamine-induced behaviors in transgenic mice lacking the trace amine-associated receptor 1". Pharmacology, Biochemistry, and Behavior. 101 (2): 201–207. doi:10.1016/j.pbb.2011.10.025. PMC 3288391. PMID 22079347.
- ^ Kuropka P, Zawadzki M, Szpot P (May 2023). "A narrative review of the neuropharmacology of synthetic cathinones-Popular alternatives to classical drugs of abuse". Hum Psychopharmacol. 38 (3): e2866. doi:10.1002/hup.2866. PMID 36866677.
Another feature that distinguishes [substituted cathinones (SCs)] from amphetamines is their negligible interaction with the trace amine associated receptor 1 (TAAR1). Activation of this receptor reduces the activity of dopaminergic neurones, thereby reducing psychostimulatory effects and addictive potential (Miller, 2011; Simmler et al., 2016). Amphetamines are potent agonists of this receptor, making them likely to self‐inhibit their stimulating effects. In contrast, SCs show negligible activity towards TAAR1 (Kolaczynska et al., 2021; Rickli et al., 2015; Simmler et al., 2014, 2016). [...] The lack of self‐regulation by TAAR1 may partly explain the higher addictive potential of SCs compared to amphetamines (Miller, 2011; Simmler et al., 2013).
- ^ Simmler LD, Liechti ME (2018). "Pharmacology of MDMA- and Amphetamine-Like New Psychoactive Substances". Handb Exp Pharmacol. Handbook of Experimental Pharmacology. 252: 143–164. doi:10.1007/164_2018_113. ISBN 978-3-030-10560-0. PMID 29633178.
The activation of human TAAR1 might diminish the effects of psychostimulation and intoxication arising from 7-APB effects on monoamine transporters (see 4.1.3. for more details). Affinity to mouse and rat TAAR1 has been shown for many psychostimulants, but species differences are common (Simmler et al. 2016). For example, [5-(2-aminopropyl)indole (5-IT)] and [4-methylamphetamine (4-MA)] bind and activate TAAR1 in the nanomolar range, but do not activate human TAAR1.
- ^ a b c Simmler LD, Buchy D, Chaboz S, Hoener MC, Liechti ME (April 2016). "In Vitro Characterization of Psychoactive Substances at Rat, Mouse, and Human Trace Amine-Associated Receptor 1". J Pharmacol Exp Ther. 357 (1): 134–144. doi:10.1124/jpet.115.229765. PMID 26791601.
- ^ Rickli A, Kolaczynska K, Hoener MC, Liechti ME (May 2019). "Pharmacological characterization of the aminorex analogs 4-MAR, 4,4'-DMAR, and 3,4-DMAR". Neurotoxicology. 72: 95–100. Bibcode:2019NeuTx..72...95R. doi:10.1016/j.neuro.2019.02.011. PMID 30776375.
- ^ a b Schmitt KC, Reith ME (2011). "The atypical stimulant and nootropic modafinil interacts with the dopamine transporter in a different manner than classical cocaine-like inhibitors". PLOS ONE. 6 (10): e25790. Bibcode:2011PLoSO...625790S. doi:10.1371/journal.pone.0025790. PMC 3197159. PMID 22043293.
- ^ Tanda G, Hersey M, Hempel B, Xi ZX, Newman AH (February 2021). "Modafinil and its structural analogs as atypical dopamine uptake inhibitors and potential medications for psychostimulant use disorder". Current Opinion in Pharmacology. 56: 13–21. doi:10.1016/j.coph.2020.07.007. PMC 8247144. PMID 32927246.
- ^ a b c d Knoll J, Miklya I, Knoll B, Markó R, Rácz D (1996). "Phenylethylamine and tyramine are mixed-acting sympathomimetic amines in the brain". Life Sciences. 58 (23): 2101–2114. doi:10.1016/0024-3205(96)00204-4. PMID 8649195.
- ^ Harsing LG, Knoll J, Miklya I (August 2022). "Enhancer Regulation of Dopaminergic Neurochemical Transmission in the Striatum". International Journal of Molecular Sciences. 23 (15): 8543. doi:10.3390/ijms23158543. PMC 9369307. PMID 35955676.
- ^ Harsing LG, Timar J, Miklya I (August 2023). "Striking Neurochemical and Behavioral Differences in the Mode of Action of Selegiline and Rasagiline". International Journal of Molecular Sciences. 24 (17): 13334. doi:10.3390/ijms241713334. PMC 10487936. PMID 37686140.
- ^ a b c d e f g h i j k l m n o p q r s t u v Rothman RB, Baumann MH, Dersch CM, Romero DV, Rice KC, Carroll FI, et al. (January 2001). "Amphetamine-type central nervous system stimulants release norepinephrine more potently than they release dopamine and serotonin". Synapse. 39 (1): 32–41. doi:10.1002/1098-2396(20010101)39:1<32::AID-SYN5>3.0.CO;2-3. PMID 11071707. S2CID 15573624.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y Blough BE, Landavazo A, Decker AM, Partilla JS, Baumann MH, Rothman RB (October 2014). "Interaction of psychoactive tryptamines with biogenic amine transporters and serotonin receptor subtypes". Psychopharmacology. 231 (21): 4135–4144. doi:10.1007/s00213-014-3557-7. PMC 4194234. PMID 24800892.
- ^ Nakamura M, Ishii A, Nakahara D (May 1998). "Characterization of beta-phenylethylamine-induced monoamine release in rat nucleus accumbens: a microdialysis study". European Journal of Pharmacology. 349 (2–3): 163–169. doi:10.1016/s0014-2999(98)00191-5. PMID 9671094.
- ^ Zsilla G, Hegyi DE, Baranyi M, Vizi ES (October 2018). "3,4-Methylenedioxymethamphetamine, mephedrone, and β-phenylethylamine release dopamine from the cytoplasm by means of transporters and keep the concentration high and constant by blocking reuptake". European Journal of Pharmacology. 837: 72–80. doi:10.1016/j.ejphar.2018.08.037. PMID 30172789.
- ^ Shulgin AT, Shulgin A (1991). Pihkal: A Chemical Love Story. Biography/science. Transform Press. ISBN 978-0-9630096-0-9. Retrieved 18 August 2024.
- ^ Shulgin AT, Shulgin A (1997). Tihkal: The Continuation. Transform Press. ISBN 978-0-9630096-9-2. Retrieved 18 August 2024.
- ^ a b c Shulgin A, Manning T, Daley PF (2011). The Shulgin Index: Psychedelic Phenethylamines and Related Compounds. Vol. 1. Transform Press. ISBN 978-0-9630096-3-0.
- ^ a b Underhill SM, Hullihen PD, Chen J, Fenollar-Ferrer C, Rizzo MA, Ingram SL, et al. (April 2021). "Amphetamines signal through intracellular TAAR1 receptors coupled to Gα13 and GαS in discrete subcellular domains". Mol Psychiatry. 26 (4): 1208–1223. doi:10.1038/s41380-019-0469-2. PMC 7038576. PMID 31399635.
Although the precise physiological role of TAAR1/G13-mediated DAT internalization remains to be established, it is likely that this pathway evolved to regulate the actions of endogenous amines including β-PEA, tyramine, 3-methoxytyramine, and DA. DA is a TAAR1 agonist (Fig. 1c) and recently, it was shown that the sustained elevation of extracellular DA seen following burst firing appears to be a consequence of DAT internalization by a Rho-dependent mechanism [51]. These results provide the first evidence that dopamine itself can act as a TAAR1 agonist to trigger transporter internalization in vivo. TAAR1 signaling also has the potential to serve as a sensor of cytoplasmic DA and its metabolites. At high cytosolic concentrations, DA becomes neurotoxic due to the formation of reactive oxygen species and quinones that can cause damage to the neuron [52]. Under normal conditions, DA transported through the DAT from the extracellular space is rapidly repackaged into synaptic vesicles or enzymatically metabolized. However, if cytoplasmic DA concentrations saturate these mechanisms, the reduction in surface levels of DAT mediated by TAAR1/G13 signaling may provide an additional means for maintaining free cytosolic DA below toxic levels.
- ^ Guillot TS, Miller GW (April 2009). "Protective actions of the vesicular monoamine transporter 2 (VMAT2) in monoaminergic neurons". Mol Neurobiol. 39 (2): 149–170. doi:10.1007/s12035-009-8059-y. PMID 19259829.
- ^ Mulvihill KG (January 2019). "Presynaptic regulation of dopamine release: Role of the DAT and VMAT2 transporters". Neurochem Int. 122: 94–105. doi:10.1016/j.neuint.2018.11.004. PMID 30465801.
- ^ Goldstein DS, Kopin IJ, Sharabi Y (December 2014). "Catecholamine autotoxicity. Implications for pharmacology and therapeutics of Parkinson disease and related disorders". Pharmacol Ther. 144 (3): 268–282. doi:10.1016/j.pharmthera.2014.06.006. PMC 4591072. PMID 24945828.
- ^ a b c Docherty JR, Alsufyani HA (August 2021). "Pharmacology of Drugs Used as Stimulants". J Clin Pharmacol. 61 Suppl 2: S53–S69. doi:10.1002/jcph.1918. PMID 34396557.
- ^ Angoa-Pérez M, Anneken JH, Kuhn DM (2017). "Neurotoxicology of Synthetic Cathinone Analogs". Curr Top Behav Neurosci. 32: 209–230. doi:10.1007/7854_2016_21. PMC 6100737. PMID 27753008.
This flooding of the cytoplasm and synaptic space with the oxidatively labile DA is thought to be a critical first step in the neurotoxic cascade of the amphetamines [73]. These conditions of elevated concentrations of cytosolic monoamines could be further aggravated by inhibition of MAO [91]. Unlike amphetamines, mephedrone and methylone have little if any affinity for VMAT-2 [33]. Therefore, their lack of neurotoxicity could derive from an inability to promote the release of DA from storage vesicles into the cytoplasm.
- ^ Pifl C, Reither H, Hornykiewicz O (May 2015). "The profile of mephedrone on human monoamine transporters differs from 3,4-methylenedioxymethamphetamine primarily by lower potency at the vesicular monoamine transporter". Eur J Pharmacol. 755: 119–126. doi:10.1016/j.ejphar.2015.03.004. PMID 25771452.
- ^ a b Kostrzewa RM (2022). "Survey of Selective Monoaminergic Neurotoxins Targeting Dopaminergic, Noradrenergic, and Serotoninergic Neurons". Handbook of Neurotoxicity. Cham: Springer International Publishing. pp. 159–198. doi:10.1007/978-3-031-15080-7_53. ISBN 978-3-031-15079-1.
- ^ a b c d Moratalla R, Khairnar A, Simola N, Granado N, García-Montes JR, Porceddu PF, et al. (August 2017). "Amphetamine-related drugs neurotoxicity in humans and in experimental animals: Main mechanisms". Prog Neurobiol. 155: 149–170. doi:10.1016/j.pneurobio.2015.09.011. hdl:10261/156486. PMID 26455459.
- ^ a b c Baumeister AA (2021). "Is Attention-Deficit/Hyperactivity Disorder a Risk Syndrome for Parkinson's Disease?" (PDF). Harv Rev Psychiatry. 29 (2): 142–158. doi:10.1097/HRP.0000000000000283. PMID 33560690.
It has been suggested that the association between PD and ADHD may be explained, in part, by toxic effects of these drugs on DA neurons.241 [...] An important question is whether amphetamines, as they are used clinically to treat ADHD, are toxic to DA neurons. In most of the animal and human studies cited above, stimulant exposure levels are high relative to clinical doses, and dosing regimens (as stimulants) rarely mimic the manner in which these drugs are used clinically. The study by Ricaurte and colleagues248 is an exception. In that study, baboons orally self-administered a racemic (3:1 d/l) amphetamine mixture twice daily in increasing doses ranging from 2.5 to 20 mg/day for four weeks. Plasma amphetamine concentrations, measured at one-week intervals, were comparable to those observed in children taking amphetamine for ADHD. Two to four weeks after cessation of amphetamine treatment, multiple markers of striatal DA function were decreased, including DA and DAT. In another group of animals (squirrel monkeys), d/l amphetamine blood concentration was titrated to clinically comparable levels for four weeks by administering varying doses of amphetamine by orogastric gavage. These animals also had decreased markers of striatal DA function assessed two weeks after cessation of amphetamine.
- ^ Asser A, Taba P (2015). "Psychostimulants and movement disorders". Front Neurol. 6: 75. doi:10.3389/fneur.2015.00075. PMC 4403511. PMID 25941511.
Amphetamine treatment similar to that used for ADHD has been demonstrated to produce brain dopaminergic neurotoxicity in primates, causing the damage of dopaminergic nerve endings in the striatum that may also occur in other disorders with long-term amphetamine treatment (57).
- ^ a b Advokat C (July 2007). "Update on amphetamine neurotoxicity and its relevance to the treatment of ADHD". J Atten Disord. 11 (1): 8–16. doi:10.1177/1087054706295605. PMID 17606768.
- ^ Berman SM, Kuczenski R, McCracken JT, London ED (February 2009). "Potential adverse effects of amphetamine treatment on brain and behavior: a review". Mol Psychiatry. 14 (2): 123–142. doi:10.1038/mp.2008.90. PMC 2670101. PMID 18698321.
Though the paradigm used by Ricaurte et al. 53 arguably still incorporates amphetamine exposure at a level above much clinical use,14,55 it raises important unanswered questions. Is there a threshold of amphetamine exposure above which persistent changes in the dopamine system are induced? [...]
- ^ Ricaurte GA, Mechan AO, Yuan J, Hatzidimitriou G, Xie T, Mayne AH, et al. (October 2005). "Amphetamine treatment similar to that used in the treatment of adult attention-deficit/hyperactivity disorder damages dopaminergic nerve endings in the striatum of adult nonhuman primates". J Pharmacol Exp Ther. 315 (1): 91–98. doi:10.1124/jpet.105.087916. PMID 16014752.
- ^ Courtney KE, Ray LA (2016). "Clinical neuroscience of amphetamine-type stimulants: From basic science to treatment development". Prog Brain Res. 223: 295–310. doi:10.1016/bs.pbr.2015.07.010. PMID 26806782.
Repeated exposure to moderate to high levels of methamphetamine has been related to neurotoxic effects on the dopaminergic and serotonergic systems, leading to potentially irreversible loss of nerve terminals and/or neuron cell bodies (Cho and Melega, 2002). Preclinical evidence suggests that d-amphetamine, even when administered at commonly prescribed therapeutic doses, also results in toxicity to brain dopaminergic axon terminals (Ricaurte et al., 2005).
- ^ Gerlach M, Grünblatt E, Lange KW (June 2013). "Is the treatment with psychostimulants in children and adolescents with attention deficit hyperactivity disorder harmful for the dopaminergic system?". Atten Defic Hyperact Disord. 5 (2): 71–81. doi:10.1007/s12402-013-0105-y. PMID 23605387.
- ^ a b c Oeri HE (May 2021). "Beyond ecstasy: Alternative entactogens to 3,4-methylenedioxymethamphetamine with potential applications in psychotherapy". J Psychopharmacol. 35 (5): 512–536. doi:10.1177/0269881120920420. PMC 8155739. PMID 32909493.
- ^ Pinterova N, Horsley RR, Palenicek T (2017). "Synthetic Aminoindanes: A Summary of Existing Knowledge". Front Psychiatry. 8: 236. doi:10.3389/fpsyt.2017.00236. PMC 5698283. PMID 29204127.
- ^ a b c d e f g h i j k l m n o p q r s t u Nagai F, Nonaka R, Satoh Hisashi Kamimura K (March 2007). "The effects of non-medically used psychoactive drugs on monoamine neurotransmission in rat brain". European Journal of Pharmacology. 559 (2–3): 132–137. doi:10.1016/j.ejphar.2006.11.075. PMID 17223101.
- ^ a b c d e f Del Bello F, Sakloth F, Partilla JS, Baumann MH, Glennon RA (September 2015). "Ethylenedioxy homologs of N-methyl-(3,4-methylenedioxyphenyl)-2-aminopropane (MDMA) and its corresponding cathinone analog methylenedioxymethcathinone: Interactions with transporters for serotonin, dopamine, and norepinephrine". Bioorg Med Chem. 23 (17): 5574–5579. doi:10.1016/j.bmc.2015.07.035. PMC 4562428. PMID 26233799.
The present findings with MDMA are consistent with our previous data [15,17] and those reported by Simmler et al. [4] and Eshleman et al. [23] who examined the effects of MDMA and related drugs in human embryonic kidney (HEK) cells transfected with human SERT, DAT and NET. Thus, the molecular mechanism of action for MDMA at monoamine transporters is similar in rats and humans. On the other hand, the potency of (±)MDMA for releasing monoamines in rat brain synaptosomes shown here (i.e., 60–70 nM) is greater than its potency in transfected HEK cells (i.e., 1–20 μM). Such discrepancies in absolute potency could be related to species differences in drug responsiveness, differences in release assay methods employed, or the absence of important neuronal membrane proteins in non-neuronal HEK cells.
- ^ Nichols DE, Oberlender R, Burris K, Hoffman AJ, Johnson MP (November 1989). "Studies of dioxole ring substituted 3,4-methylenedioxyamphetamine (MDA) analogues". Pharmacol Biochem Behav. 34 (3): 571–576. doi:10.1016/0091-3057(89)90560-1. PMID 2623014.
- ^ Nichols DE (1994). "Medicinal Chemistry and Structure–Activity Relationships". In Cho AK, Segal DS (eds.). Amphetamine and Its Analogs: Psychopharmacology, Toxicology, and Abuse. Academic Press. pp. 3–41. ISBN 978-0-12-173375-9.
- ^ a b c d e f g Brandt SD, Walters HM, Partilla JS, Blough BE, Kavanagh PV, Baumann MH (December 2020). "The psychoactive aminoalkylbenzofuran derivatives, 5-APB and 6-APB, mimic the effects of 3,4-methylenedioxyamphetamine (MDA) on monoamine transmission in male rats". Psychopharmacology (Berl). 237 (12): 3703–3714. doi:10.1007/s00213-020-05648-z. PMC 7686291. PMID 32875347.
- ^ a b Fuwa T, Suzuki J, Tanaka T, Inomata A, Honda Y, Kodama T (2016). "Novel psychoactive benzofurans strongly increase extracellular serotonin level in mouse corpus striatum". J Toxicol Sci. 41 (3): 329–337. doi:10.2131/jts.41.329. PMID 27193726.
- ^ a b c Monte AP, Marona-Lewicka D, Cozzi NV, Nichols DE (November 1993). "Synthesis and pharmacological examination of benzofuran, indan, and tetralin analogues of 3,4-(methylenedioxy)amphetamine". J Med Chem. 36 (23): 3700–3706. doi:10.1021/jm00075a027. PMID 8246240.
- ^ a b c d e f g Johnson CB, Walther D, Baggott MJ, Baker LE, Baumann MH (September 2024). "Novel Benzofuran Derivatives Induce Monoamine Release and Substitute for the Discriminative Stimulus Effects of 3,4-Methylenedioxymethamphetamine". J Pharmacol Exp Ther. 391 (1): 22–29. doi:10.1124/jpet.123.001837. PMC 11413916. PMID 38272669.
- ^ a b c d e f g h Rudin D, McCorvy JD, Glatfelter GC, Luethi D, Szöllősi D, Ljubišić T, et al. (March 2022). "Aminopropylbenzothiophenes (APBTs) are novel monoamine transporter ligands that lack stimulant effects but display psychedelic-like activity in mice". Neuropsychopharmacology. 47 (4): 914–923. doi:10.1038/s41386-021-01221-0. PMC 8882185. PMID 34750565.
- ^ Mydecine (13 June 2023). "Short-acting 3,4-methylenedioxymethamphetamine (mdma) analogs incorporating benzothiazole". Google Patents. Retrieved 23 October 2024.
- ^ a b c d Marusich JA, Antonazzo KR, Blough BE, Brandt SD, Kavanagh PV, Partilla JS, et al. (February 2016). "The new psychoactive substances 5-(2-aminopropyl)indole (5-IT) and 6-(2-aminopropyl)indole (6-IT) interact with monoamine transporters in brain tissue". Neuropharmacology. 101: 68–75. doi:10.1016/j.neuropharm.2015.09.004. PMC 4681602. PMID 26362361.
- ^ Parker MA, Marona-Lewicka D, Kurrasch D, Shulgin AT, Nichols DE (March 1998). "Synthesis and pharmacological evaluation of ring-methylated derivatives of 3,4-(methylenedioxy)amphetamine (MDA)". J Med Chem. 41 (6): 1001–1005. doi:10.1021/jm9705925. PMID 9526575.
- ^ a b c d e f g h i j k l m n Rothman RB, Partilla JS, Baumann MH, Lightfoot-Siordia C, Blough BE (April 2012). "Studies of the biogenic amine transporters. 14. Identification of low-efficacy "partial" substrates for the biogenic amine transporters". The Journal of Pharmacology and Experimental Therapeutics. 341 (1): 251–262. doi:10.1124/jpet.111.188946. PMC 3364510. PMID 22271821.
- ^ a b c d Glennon RA, Young R, Hauck AE, McKenney JD (December 1984). "Structure-activity studies on amphetamine analogs using drug discrimination methodology". Pharmacol Biochem Behav. 21 (6): 895–901. doi:10.1016/s0091-3057(84)80071-4. PMID 6522418.
- ^ a b c d e f Alberto-Silva AS, Hemmer S, Bock HA, Alves da Silva L, Scott KR, Kastner N, et al. (April 2024). "Bioisosteric analogs of MDMA with improved pharmacological profile". bioRxiv. doi:10.1101/2024.04.08.588083. PMC 11030374. PMID 38645142.
- ^ a b c d e f g h i Forsyth AN (22 May 2012). "Synthesis and Biological Evaluation of Rigid Analogues of Methamphetamines". ScholarWorks@UNO. Retrieved 4 November 2024.
- ^ a b c Decker AM, Partilla JS, Baumann MH, Rothman RB, Blough BE (2016). "The biogenic amine transporter activity of vinylogous amphetamine analogs". MedChemComm. 7 (8): 1657–1663. doi:10.1039/C6MD00245E. ISSN 2040-2503.
- ^ a b c "Vinylogous phenethylamines as neurotransmitter releasers". Google Patents. 11 May 2017. Retrieved 7 December 2024.
- ^ a b Maier J, Rauter L, Rudin D, Niello M, Holy M, Schmid D, et al. (June 2021). "α-PPP and its derivatives are selective partial releasers at the human norepinephrine transporter: A pharmacological characterization of interactions between pyrrolidinopropiophenones and high and low affinity monoamine transporters". Neuropharmacology. 190: 108570. doi:10.1016/j.neuropharm.2021.108570. PMID 33864800.
- ^ a b Eshleman AJ, Wolfrum KM, Reed JF, Kim SO, Swanson T, Johnson RA, et al. (January 2017). "Structure-Activity Relationships of Substituted Cathinones, with Transporter Binding, Uptake, and Release". J Pharmacol Exp Ther. 360 (1): 33–47. doi:10.1124/jpet.116.236349. PMC 5193076. PMID 27799294.
- ^ a b c d e f Severinsen K, Kraft JF, Koldsø H, Vinberg KA, Rothman RB, Partilla JS, et al. (September 2012). "Binding of the amphetamine-like 1-phenyl-piperazine to monoamine transporters". ACS Chem Neurosci. 3 (9): 693–705. doi:10.1021/cn300040f. PMC 3447394. PMID 23019496.
- ^ a b c d e f Halberstadt AL, Brandt SD, Walther D, Baumann MH (March 2019). "2-Aminoindan and its ring-substituted derivatives interact with plasma membrane monoamine transporters and α2-adrenergic receptors". Psychopharmacology (Berl). 236 (3): 989–999. doi:10.1007/s00213-019-05207-1. PMC 6848746. PMID 30904940.
- ^ a b c d Nichols DE, Marona-Lewicka D, Huang X, Johnson MP (1993). "Novel serotonergic agents". Drug des Discov. 9 (3–4): 299–312. PMID 8400010.
- ^ WO 2022/032147, Baggott M, "2-Aminoindane compounds for mental disorders or enhancement.", published 10 February 2022, assigned to Tactogen Inc.
- ^ Hathaway BA, Nichols DE, Nichols MB, Yim GK (May 1982). "A new, potent, conformationally restricted analogue of amphetamine: 2-amino-1,2-dihydronaphthalene". J Med Chem. 25 (5): 535–538. doi:10.1021/jm00347a011. PMID 6123601.
- ^ Oberlender R, Nichols DE (March 1991). "Structural variation and (+)-amphetamine-like discriminative stimulus properties". Pharmacol Biochem Behav. 38 (3): 581–586. doi:10.1016/0091-3057(91)90017-v. PMID 2068194.
- ^ a b c d Vekariya R (2012). "Towards Understanding the Mechanism of Action of Abused Cathinones". VCU Theses and Dissertations. doi:10.25772/AR93-7024.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x Blough BE, Decker AM, Landavazo A, Namjoshi OA, Partilla JS, Baumann MH, et al. (March 2019). "The dopamine, serotonin and norepinephrine releasing activities of a series of methcathinone analogs in male rat brain synaptosomes". Psychopharmacology. 236 (3): 915–924. doi:10.1007/s00213-018-5063-9. PMC 6475490. PMID 30341459.
- ^ a b "Specialized combinations for mental disorders or mental enhancement". Google Patents. 7 June 2024. Retrieved 4 November 2024.
- ^ a b Rickli A, Hoener MC, Liechti ME (September 2019). "Pharmacological profiles of compounds in preworkout supplements ("boosters")". Eur J Pharmacol. 859: 172515. doi:10.1016/j.ejphar.2019.172515. PMID 31265842.
- ^ a b c Docherty JR (June 2008). "Pharmacology of stimulants prohibited by the World Anti-Doping Agency (WADA)". Br J Pharmacol. 154 (3): 606–622. doi:10.1038/bjp.2008.124. PMC 2439527. PMID 18500382.
- ^ a b Delicado EG, Fideu MD, Miras-Portugal MT, Pourrias B, Aunis D (August 1990). "Effect of tuamine, heptaminol and two analogues on uptake and release of catecholamines in cultured chromaffin cells". Biochem Pharmacol. 40 (4): 821–825. doi:10.1016/0006-2952(90)90322-c. PMID 2386550.
- ^ Alsufyani HA, Docherty JR (January 2019). "Methylhexaneamine causes tachycardia and pressor responses indirectly by releasing noradrenaline in the rat". Eur J Pharmacol. 843: 121–125. doi:10.1016/j.ejphar.2018.10.047. PMID 30395850.
- ^ Catalani V, Prilutskaya M, Al-Imam A, Marrinan S, Elgharably Y, Zloh M, et al. (February 2018). "Octodrine: New Questions and Challenges in Sport Supplements". Brain Sci. 8 (2): 34. doi:10.3390/brainsci8020034. PMC 5836053. PMID 29461475.
- ^ a b Rasmussen N, Keizers PH (2016). "History full circle: 'Novel' sympathomimetics in supplements". Drug Test Anal. 8 (3–4): 283–286. doi:10.1002/dta.1852. PMID 27072841.
- ^ Venhuis BJ, de Kaste D (2012). "Scientific Opinion on the Regulatory Status of 1,3-Dimethylamylamine (DMAA)" (PDF). European Journal of Food Research & Review. 2 (4): 93–100.
- ^ Schlessinger A, Geier E, Fan H, Irwin JJ, Shoichet BK, Giacomini KM, et al. (September 2011). "Structure-based discovery of prescription drugs that interact with the norepinephrine transporter, NET". Proc Natl Acad Sci U S A. 108 (38): 15810–15815. Bibcode:2011PNAS..10815810S. doi:10.1073/pnas.1106030108. PMC 3179104. PMID 21885739.
- ^ a b c Rothman RB, Baumann MH (December 2005). "Targeted screening for biogenic amine transporters: potential applications for natural products". Life Sci. 78 (5): 512–518. doi:10.1016/j.lfs.2005.09.001. PMID 16202429.
- ^ a b c d Partilla JS, Baumann MH, Decker AM, Blough BE, Rothman RB (2016). "Interrogating the Activity of Ligands at Monoamine Transporters in Rat Brain Synaptosomes". Neurotransmitter Transporters. Vol. 118. New York, NY: Springer New York. pp. 41–52. doi:10.1007/978-1-4939-3765-3_3. ISBN 978-1-4939-3763-9.
- ^ Rothman RB, Dersch CM, Baumann MH, Carroll FI, Partilla JS (1999). "Development of a High-Throughput Assay for Biogenic Amine Transporter Substrates". Problems of Drug Dependence 1999: Proceedings of the 61st Annual Scientific Meeting, The College on Problems of Drug Dependence, Inc (PDF). NIDA Res Monogr. Vol. 180. pp. 1–476 (251). PMID 11680410.
The major goal of this study was to establish a high-throughput assay to detect [monoamine transporter substrates (SBSTs)] for use in a project to develop new drugs with dual activity as SBSTs of DAT and SERT. METHODS. Using minor modifications of published procedures, rat brain synaptosomes were preloaded with either [3H]DA, [3H]NE or [3H]5-HT. Test drugs were added and the reaction terminated by rapid filtration over Whatman GF/B filters. Release was quantified by counting how much tritium was retained on the filters. RESULTS. Using optimized conditions known SBSTs potently decreased retained tritium in a dose-dependent manner whereas known [uptake inhibitors (UIs)] were weak or ineffective. UIs shifted SBST inhibition curves to the right, consistent with antagonist-like activity. CONCLUSION. We have developed high throughput assays which detect SBSTs for the DA, 5-HT and NE transporters.
- ^ a b c d e f g h Partilla JS, Dersch CM, Baumann MH, Carroll FI, Rothman RB (1999). "Profiling CNS Stimulants with a High-Throughput Assay for Biogenic Amine Transporter Substractes". Problems of Drug Dependence 1999: Proceedings of the 61st Annual Scientific Meeting, The College on Problems of Drug Dependence, Inc (PDF). NIDA Res Monogr. Vol. 180. pp. 1–476 (252). PMID 11680410.
RESULTS. Methamphetamine and amphetamine potently released NE (IC50s = 14.3 and 7.0 nM) and DA (IC50s = 40.4 nM and 24.8 nM), and were much less potent releasers of 5-HT (IC50s = 740 nM and 1765 nM). Phentermine released all three biogenic amines with an order of potency NE (IC50 = 28.8 nM)> DA (IC50 = 262 nM)> 5-HT (IC50 = 2575 nM). Aminorex released NE (IC50 = 26.4 nM), DA (IC50 = 44.8 nM) and 5-HT (IC50 = 193 nM). Chlorphentermine was a very potent 5-HT releaser (IC50 = 18.2 nM), a weaker DA releaser (IC50 = 935 nM) and inactive in the NE release assay. Chlorphentermine was a moderate potency inhibitor of [3H]NE uptake (Ki = 451 nM). Diethylpropion, which is self-administered, was a weak DA uptake inhibitor (Ki = 15 µM) and NE uptake inhibitor (Ki = 18.1 µM) and essentially inactive in the other assays. Phendimetrazine, which is self-administered, was a weak DA uptake inhibitor (IC50 = 19 µM), a weak NE uptake inhibitor (8.3 µM) and essentially inactive in the other assays.
- ^ a b c d e f g h i j k l m n o p q r s t u Blough BE, Landavazo A, Partilla JS, Baumann MH, Decker AM, Page KM, et al. (June 2014). "Hybrid dopamine uptake blocker-serotonin releaser ligands: a new twist on transporter-focused therapeutics". ACS Med Chem Lett. 5 (6): 623–627. doi:10.1021/ml500113s. PMC 4060932. PMID 24944732.
- ^ a b Jîtcă G, Ősz BE, Tero-Vescan A, Vari CE (March 2021). "Psychoactive Drugs-From Chemical Structure to Oxidative Stress Related to Dopaminergic Neurotransmission. A Review". Antioxidants (Basel). 10 (3): 381. doi:10.3390/antiox10030381. PMC 8000782. PMID 33806320.
- ^ a b Dunlap LE, Andrews AM, Olson DE (October 2018). "Dark Classics in Chemical Neuroscience: 3,4-Methylenedioxymethamphetamine". ACS Chem Neurosci. 9 (10): 2408–2427. doi:10.1021/acschemneuro.8b00155. PMC 6197894. PMID 30001118.
- ^ a b c d e f g Maier J, Mayer FP, Brandt SD, Sitte HH (October 2018). "DARK Classics in Chemical Neuroscience: Aminorex Analogues". ACS Chem Neurosci. 9 (10): 2484–2502. doi:10.1021/acschemneuro.8b00415. PMC 6287711. PMID 30269490.
- ^ Xie Z, Miller GM (May 2008). "Beta-phenylethylamine alters monoamine transporter function via trace amine-associated receptor 1: implication for modulatory roles of trace amines in brain". J Pharmacol Exp Ther. 325 (2): 617–628. doi:10.1124/jpet.107.134247. PMID 18182557.
We confirmed that TAAR1 was activated by trace amines and demonstrated that TAAR1 activation by β-PEA significantly inhibited uptake and induced efflux of [3H]dopamine, [3H]norepinephrine, and [3H]serotonin in transfected cells. In brain synaptosomes, β-PEA significantly inhibited uptake and induced efflux of [3H]dopamine and [3H]serotonin in striatal and [3H]norepinephrine in thalamic synaptosomes of rhesus monkeys and wild-type mice, but it lacked the same effects in synaptosomes of TAAR1 knockout mice.
- ^ a b c d e f g h i j k l m n o p Walther D, Shalabi AR, Baumann MH, Glennon RA (January 2019). "Systematic Structure-Activity Studies on Selected 2-, 3-, and 4-Monosubstituted Synthetic Methcathinone Analogs as Monoamine Transporter Releasing Agents". ACS Chem Neurosci. 10 (1): 740–745. doi:10.1021/acschemneuro.8b00524. PMC 8269283. PMID 30354055.
- ^ Baggott M (21 January 2022). "[Comment]".
I measured DA and 5-HT release in vitro and [2-FMA] basically didn't release 5-HT (EC50s were around 90 nM at DAT and 15000 nM at SERT).
- ^ Baggott M (30 April 2024). "[Comment]".
[2-FMA is] a potent substrate-type releaser at NET and DAT (EC50s below 100 nM) but not SERT. [...] It's my own (Tactogen's, really) unpublished data. I assayed it while trying to understand the Borax combo.
- ^ a b c Mayer FP, Burchardt NV, Decker AM, Partilla JS, Li Y, McLaughlin G, et al. (May 2018). "Fluorinated phenmetrazine "legal highs" act as substrates for high-affinity monoamine transporters of the SLC6 family". Neuropharmacology. 134 (Pt A): 149–157. doi:10.1016/j.neuropharm.2017.10.006. PMC 7294773. PMID 28988906.
- ^ a b c d McLaughlin G, Baumann MH, Kavanagh PV, Morris N, Power JD, Dowling G, et al. (September 2018). "Synthesis, analytical characterization, and monoamine transporter activity of the new psychoactive substance 4-methylphenmetrazine (4-MPM), with differentiation from its ortho- and meta- positional isomers". Drug Test Anal. 10 (9): 1404–1416. doi:10.1002/dta.2396. PMC 7316143. PMID 29673128.
- ^ a b c d e f g h i j "Phenylmorpholines and analogues thereof". Google Patents. 20 May 2011. Retrieved 7 December 2024.
- ^ a b c Cozzi NV, Brandt SD, Daley PF, Partilla JS, Rothman RB, Tulzer A, et al. (January 2013). "Pharmacological examination of trifluoromethyl ring-substituted methcathinone analogs". Eur J Pharmacol. 699 (1–3): 180–187. doi:10.1016/j.ejphar.2012.11.008. PMC 3656655. PMID 23178523.
- ^ a b c Cozzi NV, Daley PF, Evans DL, Partilla JS, Rothman RB, Ruoho AE, et al. (2011). "Trifluoromethyl ring-substituted methcathinone analogs: activity at monoamine uptake transporters". The FASEB Journal. 25 (S1). doi:10.1096/fasebj.25.1_supplement.1083.1. ISSN 0892-6638.
- ^ a b c d e f Eshleman AJ, Forster MJ, Wolfrum KM, Johnson RA, Janowsky A, Gatch MB (March 2014). "Behavioral and neurochemical pharmacology of six psychoactive substituted phenethylamines: mouse locomotion, rat drug discrimination and in vitro receptor and transporter binding and function". Psychopharmacology (Berl). 231 (5): 875–888. doi:10.1007/s00213-013-3303-6. PMC 3945162. PMID 24142203.
- ^ a b c d e f g h i j k Shalabi AR (14 December 2017). Structure-Activity Relationship Studies of Bupropion and Related 3-Substituted Methcathinone Analogues at Monoamine Transporters. VCU Scholars Compass (Thesis). doi:10.25772/M4E1-3549. Retrieved 24 November 2024.
- ^ a b "Norfenfluramine to treat dravet syndrome". Google Patents. 9 March 2023. Retrieved 7 December 2024.
- ^ a b c Shalabi AR, Walther D, Baumann MH, Glennon RA (June 2017). "Deconstructed Analogues of Bupropion Reveal Structural Requirements for Transporter Inhibition versus Substrate-Induced Neurotransmitter Release". ACS Chem Neurosci. 8 (6): 1397–1403. doi:10.1021/acschemneuro.7b00055. PMC 7261150. PMID 28220701.
- ^ Carroll FI, Blough BE, Mascarella SW, Navarro HA, Lukas RJ, Damaj MI (2014). "Bupropion and bupropion analogs as treatments for CNS disorders". Emerging Targets & Therapeutics in the Treatment of Psychostimulant Abuse. Adv Pharmacol. Vol. 69. pp. 177–216. doi:10.1016/B978-0-12-420118-7.00005-6. ISBN 978-0-12-420118-7. PMID 24484978.
- ^ a b Namjoshi OA, Decker AM, Landavazo A, Partilla JS, Baumann MH, Rothman RB, et al. (2015). "Chemical modifications to alter monoamine releasing activity of phenmetrazine analogs as potential treatments of stimulant addiction". Drug and Alcohol Dependence. 146: e48. doi:10.1016/j.drugalcdep.2014.09.502.
- ^ Kohut SJ, Fivel PA, Blough BE, Rothman RB, Mello NK (October 2013). "Effects of methcathinone and 3-Cl-methcathinone (PAL-434) in cocaine discrimination or self-administration in rhesus monkeys". Int J Neuropsychopharmacol. 16 (9): 1985–1998. doi:10.1017/S146114571300059X. PMID 23768644.
- ^ a b c d Wee S, Anderson KG, Baumann MH, Rothman RB, Blough BE, Woolverton WL (May 2005). "Relationship between the serotonergic activity and reinforcing effects of a series of amphetamine analogs". The Journal of Pharmacology and Experimental Therapeutics. 313 (2): 848–854. doi:10.1124/jpet.104.080101. PMID 15677348. S2CID 12135483.
- ^ Negus SS, Baumann MH, Rothman RB, Mello NK, Blough BE (April 2009). "Selective suppression of cocaine- versus food-maintained responding by monoamine releasers in rhesus monkeys: benzylpiperazine, (+)phenmetrazine, and 4-benzylpiperidine". J Pharmacol Exp Ther. 329 (1): 272–281. doi:10.1124/jpet.108.143701. PMC 2670586. PMID 19151247.
- ^ a b c d e Baumann MH, Walters HM, Niello M, Sitte HH (2018). "Neuropharmacology of Synthetic Cathinones". Handb Exp Pharmacol. Handbook of Experimental Pharmacology. 252: 113–142. doi:10.1007/164_2018_178. ISBN 978-3-030-10560-0. PMC 7257813. PMID 30406443.
- ^ a b c d e f g h i j k Sakloth F (11 December 2015). Psychoactive synthetic cathinones (or 'bath salts'): Investigation of mechanisms of action. VCU Scholars Compass (Thesis). doi:10.25772/AY8R-PW77. Retrieved 24 November 2024.
- ^ a b c d e f Bonano JS, Banks ML, Kolanos R, Sakloth F, Barnier ML, Glennon RA, et al. (May 2015). "Quantitative structure-activity relationship analysis of the pharmacology of para-substituted methcathinone analogues". Br J Pharmacol. 172 (10): 2433–2444. doi:10.1111/bph.13030. PMC 4409897. PMID 25438806.
- ^ a b c d e f g h i j Fitzgerald LR, Gannon BM, Walther D, Landavazo A, Hiranita T, Blough BE, et al. (March 2024). "Structure-activity relationships for locomotor stimulant effects and monoamine transporter interactions of substituted amphetamines and cathinones". Neuropharmacology. 245: 109827. doi:10.1016/j.neuropharm.2023.109827. PMC 10842458. PMID 38154512.
- ^ a b c d Nicole L (2022). "In vivo Structure-Activity Relationships of Substituted Amphetamines and Substituted Cathinones". ProQuest. Retrieved 5 December 2024.
FIGURE 2-6: Release: Effects of the specified test drug on monoamine release by DAT (red circles), NET (blue squares), and SERT (black traingles) in rat brain tissue. [...] EC50 values determined for the drug indicated within the panel. [...]
- ^ a b c Brandt SD, Baumann MH, Partilla JS, Kavanagh PV, Power JD, Talbot B, et al. (2014). "Characterization of a novel and potentially lethal designer drug (±)-cis-para-methyl-4-methylaminorex (4,4'-DMAR, or 'Serotoni')". Drug Testing and Analysis. 6 (7–8): 684–695. doi:10.1002/dta.1668. PMC 4128571. PMID 24841869.
- ^ a b c d Solis E, Partilla JS, Sakloth F, Ruchala I, Schwienteck KL, De Felice LJ, et al. (September 2017). "N-Alkylated Analogs of 4-Methylamphetamine (4-MA) Differentially Affect Monoamine Transporters and Abuse Liability". Neuropsychopharmacology. 42 (10): 1950–1961. doi:10.1038/npp.2017.98. PMC 5561352. PMID 28530234.
- ^ Huang X, Marona-Lewicka D, Nichols DE (December 1992). "p-methylthioamphetamine is a potent new non-neurotoxic serotonin-releasing agent". Eur J Pharmacol. 229 (1): 31–38. doi:10.1016/0014-2999(92)90282-9. PMID 1473561.
- ^ Sotomayor-Zárate R, Quiroz G, Araya KA, Abarca J, Ibáñez MR, Montecinos A, et al. (December 2012). "4-Methylthioamphetamine increases dopamine in the rat striatum and has rewarding effects in vivo". Basic Clin Pharmacol Toxicol. 111 (6): 371–379. doi:10.1111/j.1742-7843.2012.00926.x. PMID 22788961.
- ^ a b c Simmler LD, Rickli A, Hoener MC, Liechti ME (April 2014). "Monoamine transporter and receptor interaction profiles of a new series of designer cathinones". Neuropharmacology. 79: 152–160. doi:10.1016/j.neuropharm.2013.11.008. PMID 24275046.
- ^ a b c d e f g h i j k Glennon RA, Dukat M (2017). "Structure-Activity Relationships of Synthetic Cathinones". Curr Top Behav Neurosci. Current Topics in Behavioral Neurosciences. 32: 19–47. doi:10.1007/7854_2016_41. ISBN 978-3-319-52442-9. PMC 5818155. PMID 27830576.
- ^ a b c Glennon RA (April 2017). "The 2014 Philip S. Portoghese Medicinal Chemistry Lectureship: The "Phenylalkylaminome" with a Focus on Selected Drugs of Abuse". J Med Chem. 60 (7): 2605–2628. doi:10.1021/acs.jmedchem.7b00085. PMC 5824997. PMID 28244748.
Table 5. Action of MDMA, MDA, and PMMA as Releasing Agents at the Serotonin (SERT), Dopamine (DAT), and Norepinephrine (NET) Transporters18,59,60 [...] a Data, although from different publications, were obtained from the same laboratory.
- ^ a b c d McLaughlin G, Morris N, Kavanagh PV, Power JD, Twamley B, O'Brien J, et al. (July 2015). "Synthesis, characterization, and monoamine transporter activity of the new psychoactive substance 3',4'-methylenedioxy-4-methylaminorex (MDMAR)". Drug Testing and Analysis. 7 (7): 555–564. doi:10.1002/dta.1732. PMC 5331736. PMID 25331619.
- ^ a b c d e f Fantegrossi WE, Gannon BM (September 2024). "A "Furious" Effort to Develop Novel 3,4-Methylenedioxymethamphetamine-Like Therapeutics". J Pharmacol Exp Ther. 391 (1): 18–21. doi:10.1124/jpet.124.002183. PMID 39293859.
- ^ a b c "Advantageous benzofuran compositions for mental disorders or enhancement". Google Patents. 8 December 2022. Retrieved 21 November 2024.
- ^ a b Davies RA, Baird TR, Nguyen VT, Ruiz B, Sakloth F, Eltit JM, et al. (June 2020). "Investigation of the Optical Isomers of Methcathinone, and Two Achiral Analogs, at Monoamine Transporters and in Intracranial Self-Stimulation Studies in Rats". ACS Chem Neurosci. 11 (12): 1762–1769. doi:10.1021/acschemneuro.9b00617. PMC 10019599. PMID 32356961.
- ^ a b Nguyen V (2019). "Analyzing Interactions Between Methcathinone Analogs and the Human Monoamine Transporters". VCU Theses and Dissertations. doi:10.25772/T1DW-MG60.
- ^ a b c d Davies RA (10 July 2019). Structure-Activity Relationship Studies of Synthetic Cathinones and Related Agents. VCU Scholars Compass (Thesis). doi:10.25772/TZSA-0396. Retrieved 24 November 2024.
- ^ Blough B, Landavazo T, Partilla JS, Page KM, Rothman RB (June 2007). The Biogenic Amine Transporter Properties of Selected Shulgin Tryptamines (Abstract 50). 69th CPDD Annual Scientific Meeting. Quebec City, Quebec, Canada: College on Problems of Drug Dependence.
- ^ a b c Yadav BJ (16 July 2019). Understanding Structure–Activity Relationship of Synthetic Cathinones (Bath Salts) Utilizing Methylphenidate. VCU Scholars Compass (Thesis). doi:10.25772/MJQW-8C64. Retrieved 24 November 2024.
- ^ a b Yu H, Rothman RB, Dersch CM, Partilla JS, Rice KC (December 2000). "Uptake and release effects of diethylpropion and its metabolites with biogenic amine transporters". Bioorganic & Medicinal Chemistry. 8 (12): 2689–2692. doi:10.1016/s0968-0896(00)00210-8. PMID 11131159.
- ^ a b c d Baumann MH, Partilla JS, Lehner KR, Thorndike EB, Hoffman AF, Holy M, et al. (March 2013). "Powerful cocaine-like actions of 3,4-methylenedioxypyrovalerone (MDPV), a principal constituent of psychoactive 'bath salts' products". Neuropsychopharmacology. 38 (4): 552–562. doi:10.1038/npp.2012.204. PMC 3572453. PMID 23072836.
- ^ Liu Y (28 March 2018). "Structural Determinants for Inhibitor Recognition by the Dopamine Transporter". Duquesne Scholarship Collection. Retrieved 11 December 2024.
The most commonly studied DAT substrates are amphetamines, including amphetamine and methamphetamine (Fig. 9). S-(+)-amphetamine releases dopamine with an EC50 of 8.7 nM; the R-(−)-amphetamine is 3-fold weaker, at 27.7 nM (EC50) (Blough, Page et al. 2005). Although weaker, a similar trend is seen for the optical isomers of methamphetamine. S-(+)-methamphetamine releases dopamine with an EC50 of 24.5 nM, while the R-(−)-methamphetamine is 16-fold less active at 416 nM (EC50) (Blough, Page et al. 2005). [...] Blough, B. E., K. M. Page, et al. (2005). "Struture-activity relationship studies of DAT, SERT, and NET releasers." New Perspectives on Neurotransmitter Transporter Pharmacology.
- ^ Blough BE, Page KM, Partilla JS, Budzynski AG, Rothman RB (2005). Structure–activity relationship studies of DAT, SERT, and NET releasers. New Perspectives on Neurotransmitter Transporter Pharmacology. Alexandria, VA.
- ^ a b Baumann MH, Clark RD, Budzynski AG, Partilla JS, Blough BE, Rothman RB (March 2005). "N-substituted piperazines abused by humans mimic the molecular mechanism of 3,4-methylenedioxymethamphetamine (MDMA, or 'Ecstasy')". Neuropsychopharmacology. 30 (3): 550–560. doi:10.1038/sj.npp.1300585. PMID 15496938.
- ^ a b Baumann MH, Clark RD, Budzynski AG, Partilla JS, Blough BE, Rothman RB (October 2004). "Effects of "Legal X" piperazine analogs on dopamine and serotonin release in rat brain". Ann N Y Acad Sci. 1025 (1): 189–197. Bibcode:2004NYASA1025..189B. doi:10.1196/annals.1316.024. PMID 15542717.
- ^ a b c "Advantageous tryptamine compositions for mental disorders or enhancement". Google Patents. 20 September 2021. Retrieved 11 November 2024.
- ^ a b c Schindler CW, Thorndike EB, Rice KC, Partilla JS, Baumann MH (June 2019). "The Supplement Adulterant β-Methylphenethylamine Increases Blood Pressure by Acting at Peripheral Norepinephrine Transporters". J Pharmacol Exp Ther. 369 (3): 328–336. doi:10.1124/jpet.118.255976. PMC 6533570. PMID 30898867.
- ^ a b Saha K, Li Y, Holy M, Lehner KR, Bukhari MO, Partilla JS, et al. (March 2019). "The synthetic cathinones, butylone and pentylone, are stimulants that act as dopamine transporter blockers but 5-HT transporter substrates". Psychopharmacology (Berl). 236 (3): 953–962. doi:10.1007/s00213-018-5075-5. PMC 6476708. PMID 30345459.
- ^ Eshleman AJ, Wolfrum KM, Hatfield MG, Johnson RA, Murphy KV, Janowsky A (June 2013). "Substituted methcathinones differ in transporter and receptor interactions". Biochem Pharmacol. 85 (12): 1803–1815. doi:10.1016/j.bcp.2013.04.004. PMC 3692398. PMID 23583454.
- ^ a b c d e Hutsell BA, Baumann MH, Partilla JS, Banks ML, Vekariya R, Glennon RA, et al. (February 2016). "Abuse-related neurochemical and behavioral effects of cathinone and 4-methylcathinone stereoisomers in rats". Eur Neuropsychopharmacol. 26 (2): 288–297. doi:10.1016/j.euroneuro.2015.12.010. PMC 5331761. PMID 26738428.
- ^ a b c d e f g h i Rothman RB, Vu N, Partilla JS, Roth BL, Hufeisen SJ, Compton-Toth BA, et al. (October 2003). "In vitro characterization of ephedrine-related stereoisomers at biogenic amine transporters and the receptorome reveals selective actions as norepinephrine transporter substrates". The Journal of Pharmacology and Experimental Therapeutics. 307 (1): 138–145. doi:10.1124/jpet.103.053975. PMID 12954796. S2CID 19015584.
- ^ a b c Schindler CW, Thorndike EB, Partilla JS, Rice KC, Baumann MH (January 2021). "Amphetamine-like Neurochemical and Cardiovascular Effects of α-Ethylphenethylamine Analogs Found in Dietary Supplements". J Pharmacol Exp Ther. 376 (1): 118–126. doi:10.1124/jpet.120.000129. PMC 7788351. PMID 33082158.
- ^ a b c d Glatfelter GC, Walther D, Evans-Brown M, Baumann MH (April 2021). "Eutylone and Its Structural Isomers Interact with Monoamine Transporters and Induce Locomotor Stimulation". ACS Chem Neurosci. 12 (7): 1170–1177. doi:10.1021/acschemneuro.0c00797. PMC 9423000. PMID 33689284.
- ^ a b Costa JL, Cunha KF, Lanaro R, Cunha RL, Walther D, Baumann MH (March 2019). "Analytical quantification, intoxication case series, and pharmacological mechanism of action for N-ethylnorpentylone (N-ethylpentylone or ephylone)". Drug Test Anal. 11 (3): 461–471. doi:10.1002/dta.2502. PMC 7316160. PMID 30207090.
- ^ a b c d e f Rothman RB, Clark RD, Partilla JS, Baumann MH (June 2003). "(+)-Fenfluramine and its major metabolite, (+)-norfenfluramine, are potent substrates for norepinephrine transporters". The Journal of Pharmacology and Experimental Therapeutics. 305 (3): 1191–1199. doi:10.1124/jpet.103.049684. PMID 12649307. S2CID 21164342.
- ^ a b c d e f g h Setola V, Hufeisen SJ, Grande-Allen KJ, Vesely I, Glennon RA, Blough B, et al. (June 2003). "3,4-methylenedioxymethamphetamine (MDMA, "Ecstasy") induces fenfluramine-like proliferative actions on human cardiac valvular interstitial cells in vitro". Molecular Pharmacology. 63 (6): 1223–1229. doi:10.1124/mol.63.6.1223. PMID 12761331. S2CID 839426.
- ^ a b Rothman RB, Baumann MH (July 2002). "Therapeutic and adverse actions of serotonin transporter substrates". Pharmacology & Therapeutics. 95 (1): 73–88. doi:10.1016/s0163-7258(02)00234-6. PMID 12163129.
- ^ a b Baumann MH, Partilla JS, Ayestas MA, Page KM, Blough BE (June 2006). Eisenberg R (ed.). Interaction of MDMA and its Metabolites at Monoamine Transporters in Rat Brain (Abstract 60) (PDF). 68th Annual Scientific Meeting of The College on Problems of Drug Dependence, June 17-22, 2006, Fairmont Scottsdale Princess, Scottsdale, Arizona. p. 15.
As expected, MDMA was a potent substrate at SERT (90±7 nM) and DAT (249±19 nM). HHMA was a potent DAT substrate (130±6 nM) but weaker at SERT (1729 ±134). HMMA displayed weak activity at both SERT (607±50 nM) and DAT (3652±252 nM).
- ^ a b c d Elmore JS, Dillon-Carter O, Partilla JS, Ellefsen KN, Concheiro M, Suzuki M, et al. (February 2017). "Pharmacokinetic Profiles and Pharmacodynamic Effects for Methylone and Its Metabolites in Rats". Neuropsychopharmacology. 42 (3): 649–660. doi:10.1038/npp.2016.213. PMC 5240186. PMID 27658484.
- ^ a b Yubero-Lahoz S, Ayestas MA, Blough BE, Partilla JS, Rothman RB, de la Torre R, et al. (January 2012). "Effects of MDMA and related analogs on plasma 5-HT: relevance to 5-HT transporters in blood and brain". Eur J Pharmacol. 674 (2–3): 337–344. doi:10.1016/j.ejphar.2011.10.033. PMC 3253888. PMID 22079770.
- ^ a b Seddik A, Holy M, Weissensteiner R, Zdrazil B, Sitte HH, Ecker GF (June 2013). "Probing the Selectivity of Monoamine Transporter Substrates by Means of Molecular Modeling". Mol Inform. 32 (5–6): 409–413. doi:10.1002/minf.201300013. PMC 3743209. PMID 23956802.
- ^ Rothman RB, Baumann MH (April 2002). "Serotonin releasing agents. Neurochemical, therapeutic and adverse effects". Pharmacology, Biochemistry, and Behavior. 71 (4): 825–836. doi:10.1016/s0091-3057(01)00669-4. PMID 11888573. S2CID 24296122.
- ^ a b c d Baumann MH, Ayestas MA, Partilla JS, Sink JR, Shulgin AT, Daley PF, et al. (April 2012). "The designer methcathinone analogs, mephedrone and methylone, are substrates for monoamine transporters in brain tissue". Neuropsychopharmacology. 37 (5): 1192–1203. doi:10.1038/npp.2011.304. PMC 3306880. PMID 22169943.
- ^ a b Gregg RA, Baumann MH, Partilla JS, Bonano JS, Vouga A, Tallarida CS, et al. (February 2015). "Stereochemistry of mephedrone neuropharmacology: enantiomer-specific behavioural and neurochemical effects in rats". Br J Pharmacol. 172 (3): 883–894. doi:10.1111/bph.12951. PMC 4301696. PMID 25255824.
- ^ Gruner JA, Mathiasen JR, Flood DG, Gasior M (May 2011). "Characterization of pharmacological and wake-promoting properties of the dopaminergic stimulant sydnocarb in rats". J Pharmacol Exp Ther. 337 (2): 380–90. doi:10.1124/jpet.111.178947. PMID 21300706.
- ^ Tuv SS, Bergh MS, Andersen JM, Steinsland S, Vindenes V, Baumann MH, et al. (November 2021). "Comparative Neuropharmacology and Pharmacokinetics of Methamphetamine and Its Thiophene Analog Methiopropamine in Rodents". Int J Mol Sci. 22 (21): 12002. doi:10.3390/ijms222112002. PMC 8585037. PMID 34769427.
- ^ Iversen L, Gibbons S, Treble R, Setola V, Huang XP, Roth BL (January 2013). "Neurochemical profiles of some novel psychoactive substances". Eur J Pharmacol. 700 (1–3): 147–151. doi:10.1016/j.ejphar.2012.12.006. PMC 3582025. PMID 23261499.
- ^ Luethi D, Kaeser PJ, Brandt SD, Krähenbühl S, Hoener MC, Liechti ME (May 2018). "Pharmacological profile of methylphenidate-based designer drugs" (PDF). Neuropharmacology. 134 (Pt A): 133–140. doi:10.1016/j.neuropharm.2017.08.020. PMID 28823611.
- ^ McLaughlin G, Morris N, Kavanagh PV, Power JD, Dowling G, Twamley B, et al. (March 2017). "Synthesis, characterization and monoamine transporter activity of the new psychoactive substance mexedrone and its N-methoxy positional isomer, N-methoxymephedrone". Drug Test Anal. 9 (3): 358–368. doi:10.1002/dta.2053. PMC 5336524. PMID 27524685.
- ^ Rothman RB, Blough BE, Woolverton WL, Anderson KG, Negus SS, Mello NK, et al. (June 2005). "Development of a rationally designed, low abuse potential, biogenic amine releaser that suppresses cocaine self-administration". The Journal of Pharmacology and Experimental Therapeutics. 313 (3): 1361–1369. doi:10.1124/jpet.104.082503. PMID 15761112. S2CID 19802702.
- ^ Mayer FP, Wimmer L, Dillon-Carter O, Partilla JS, Burchardt NV, Mihovilovic MD, et al. (September 2016). "Phase I metabolites of mephedrone display biological activity as substrates at monoamine transporters". Br J Pharmacol. 173 (17): 2657–2668. doi:10.1111/bph.13547. PMC 4978154. PMID 27391165.
- ^ a b Kohut SJ, Jacobs DS, Rothman RB, Partilla JS, Bergman J, Blough BE (December 2017). "Cocaine-like discriminative stimulus effects of "norepinephrine-preferring" monoamine releasers: time course and interaction studies in rhesus monkeys". Psychopharmacology. 234 (23–24): 3455–3465. doi:10.1007/s00213-017-4731-5. PMC 5747253. PMID 28889212.
- ^ a b Glennon RA, Young R (5 August 2011). "Drug Discrimination and Mechanisms of Drug Action". Drug Discrimination. Wiley. pp. 183–216. doi:10.1002/9781118023150.ch6. ISBN 978-0-470-43352-2.
PMMA is a 5-HT releasing agent. S(+)PMMA is a potent releaser of 5-HT (EC50 = 41 nM) and NE (EC50 = 147 nM) with reduced activity as a releaser of DA (EC50 = 1,000 nM); the R(−)isomer of PMMA is a releaser of 5-HT (EC50 = 134 nM) with reduced potency for release of NE (EC50 = 1,600 nM) and DA (EC50 > 14,000 nM) (R.B. Rothman, unpublished data).
- ^ a b c Rothman RB, Katsnelson M, Vu N, Partilla JS, Dersch CM, Blough BE, et al. (June 2002). "Interaction of the anorectic medication, phendimetrazine, and its metabolites with monoamine transporters in rat brain". European Journal of Pharmacology. 447 (1): 51–57. doi:10.1016/s0014-2999(02)01830-7. PMID 12106802.
External links
[edit] Media related to Monoamine releasing agents at Wikimedia Commons
Media related to Monoamine releasing agents at Wikimedia Commons